Table of Contents
Preface
This handbook is designed to assist housestaff with common pediatric problems. This edition represents the fifth major revision. Changes to this edition include new chapters on antibiotics, skin and soft tissue infections, neonatal sepsis, intra-abdominal infections, central line infections, ALTE/BRUE, diabetes insipidus, physical and sexual abuse, diarrhea, anemia, and headache. In addition, some chapters have been condensed, revised, or expanded to provide a more accurate resource. Finally, every attempt has been made to provide an up-to-date reference, yet medicine is rapidly changing and what is standard of care today, may be ÒarchaicÓ in a few years. Thus, when in doubt, always consult other sources or your attending.
Sincere thanks to the following people, in addition to those who have previously contributed to this handbook, for their assistance with this edition:
Kathryn Stephenson, M.D.
Matthew Garber, M.D.
Scott Carney, M.D.
Melanie Blackburn, M.D..
Rathna Amarnath, M.D.
Kelly Lewis, R.D.
Dan Brown, M.D.
Jamie Parrott, M.D.
Laura Szadek, APRN, DNP, CPNP
Robert Holleman, M.D.
Anna-Kathryn Burch, M.D.
Rob Daniels, PharmD
Ron Neuberg, M.D.
Carla Roberts, M.D.
Laura Pirich, M.D.
James French, M.D.
Shilpa Shivakumar, M.D.
Derrick Wenning, M.D.
Matthew Marcus, M.D.
(TENTH EDITION)
General Pediatrics/Miscellaneous
Fluids and Electrolytes
GENERAL PRINCIPLES
- Total body water
(TBW) as a % of body water decreases with age. TBW is comprised of the intracellular (2/3) and
extracellular (1/3) compartments.
- TBW equals
¯ Birth: 80% of body
weight
¯ 6 mo: 75%
¯ 1-15 yr: 65%
¯ Adult: 50-60%
MAINTENANCE REQUIREMENTS
- Calculation by Surface Area
¯ Water:
1500-1800 ml/m²/day
¯ Na+:
30-60 mEq/m²/day
¯ K+:
20-40 mEq/m²/day
- Calculation by Weight
¯ Water:
o
0-10 kg = 100
ml/kg/day
o 11-20 kg = 1000ml + 50 ml/kg over 10 kg
o >20 kg = 1500 ml + 20 ml/kg over 20 kg
¯ Na+: 3-4
mEq/kg/day
¯ K+: 1-2 mEq/kg/day
ASSESSMENT OF
DEHYDRATION
|
Sign and Symptoms |
² 5% |
10% |
15% |
|
Decreased fluid intake |
↓ |
↓↓ |
↓↓↓↓ |
|
Postural pulse change |
No change |
↑ ³ 10 beats/min |
↑↑↑↑ |
|
Postural DBP change |
No change |
↓ ³ 10 mmHg |
↓↓↓ or frank
hypotension |
|
Fontanel/skin turgor |
Normal |
↓ |
↓↓ |
|
Mucous membranes |
Normal |
Dry |
Very dry |
|
Tears |
Present |
Reduced |
|
|
Urine output |
Normal/slight decrease |
Oliguria |
Severe oliguria or anuria |
|
Urine SG |
Normal |
↑ |
↑↑ |
|
BUN |
Normal |
↑ |
↑↑ |
|
Urine Na/FENa |
Normal |
↓ |
↓↓↑ |
|
Hct/Albumin |
Normal |
↑ |
↑↑ |
HYPOTONIC AND ISOTONIC
DEHYDRATION
For hypotonic (Na < 130) or isotonic (Na 130-150)
dehydration, rehydrate over 24 hours
á
Give 50% over the
first 8 hours, then the remainder over 16 hours
Calculate fluid and electrolyte replacement as follows:
Water Replacement
- Maintenance +
Deficit = Total water needed.
- Wt1 =
present wt in Kg,
Wt2 = calculated rehydrated weight
- Deficit: PtÕs Wt2 = Wt1/(100 -
% dehydration)
- Rehydrated
weight (Wt2) – present weight (Wt1) = deficit
water (1g = 1 mL)
Sodium Replacement
- Maintenance Na +
Deficit Na + Corrected Na (hypotonic only) = total Na needed in mEq for
the next 24 hours.
- Maintenance
sodium: 3-4 mEq/kg/day or 30-60mEq/m2/day
- Deficit
Sodium: Assume water loss is
isotonic.
- Deficit Na =
140 mEq/L x (water loss in L)
- Corrected
Sodium: (135-actual Na in mEq/L) x 0.6L/kg x (Wt in kg)
- Determine
appropriate tonicity of fluid in mEq/L =
- (Total Na
needed for 24 hrs in mEq)/(Total water needed
for 24 hrs in L)
- **Normal saline = 0.9% NaCl = 154
mEq/L NaCl (1/2NS = 77 mEq/L, etc)
- ** Psudohyponatremia: in hyperglycemia
- True Na = measured Na + 1.6 (glucose
-100)/100
Potassium Replacement
|
If not acidotic (HCO3- >18) |
If acidotic (HCO3- < 18) |
|
K < 3.5 ˆ give 40 mEq/L |
K <4 ˆ give 40
mEq/L |
|
K 3.5-5 ˆ give 20
mEq/L |
K 4-5 ˆ give 30
mEq/L |
|
K >5 ˆ give none
initially |
K 5-6 ˆ give 20
mEq/L |
|
|
K >6 ˆ give none
initially |
Example:
8 kg child who at 0.4 m² is
clinically 8% dehydrated, admission sodium is 125.
- Maintenance water: (1500)(0.4) = 600cc
- Rehydrated
weight: 8 kg/(100-8%) = 8 kg/0.92
= 8.7 kg
- Water
deficit: 8.7 kg - 8.0 kg =
0.7L or 700cc
- Total water
needed = 600cc + 700cc= 1300cc or 1.3L
- Maintenance
sodium = (40mEq/m2)(0.4m²)
= 16 mEq
- Corrected sodium
= (135mEq/L-125mEq/L)(0.6L/kg)(8kg) = 48 mEq
- Deficit sodium =
(140 mEq/L)x(0.7L) = 98 mEq
- Total sodium
required = 16 + 48 + 98 = 162 mEq
- Fluid
concentration = 162mEq/1.3L = 124 mEq/L = approximately 0.75 NS
- Order written as
follows:
D5 0.75 NS at 81 cc/hr x 8 hours, then 40 cc/hr x 16 hours - This calculation does not address
potassium needs – see above re: amount of KCl needed
HYPERTONIC DEHYDRATION
Hypertonic dehydration is corrected slowly at a uniform
rate over 48 hours with D5 0.2 to D5 0.45 NS. If re-hydrated too quickly, there is a
risk of cerebral edema. Monitor
sodium closely.
METABOLIC ACIDOSIS
If initial HCO3 < 12 then replace as follows:
á
(12 – serum
bicarb in mEq/L) x (0.6 L H2O/kg) x (Wt in kg) = mEq of NaHCO3
needed
á
Administer over 8
hours.
á
Remember that for
every mEq HCO3, a mEq of Na is given. Account for this in
calculating sodium needs.
SYMPTOMATIC HYPONATREMIA
Severe hyponatremia can lead to mental status changes and
seizures. Symptomatic hyponatremia
should be corrected with 3% saline. Goal is to rapidly increase Na to >125
to prevent seizures, then slowly correct to normal.
- (125 –
serum Na in mEq/L) x (weight in kg) x (0.6 L/kg) = mEq of Na needed
- 3 % saline =
0.513 mEq Na/mL (513 mEq/L).
- In an emergent
situation, 12cc/kg of 3% saline should raise the sodium by 10
- Administer 3%
saline over 10-15 minutes, preferably
via central IV access
HYPOMAGNESEMIA
- Replete if magnesium level
< 1 mg/dL
- Use magnesium
sulfate (50% solution), 25-50 mg/kg IV over at least 1 hr
- Max dose 2g
INTERPRETING AND CORRECTING POTASSIUM LEVELS
Considerations in interpreting K level:
á
Acid/base status:
acidosis draws intracellular K out into serum, will elevate K level but this
leads to K diuresis and loss of total body K
á
UOP: oliguria makes
higher K concerning – will not be able to regulate serum K as well
á
EKG findings: high K
will cause peaked T waves, then widened QRS, then v-tach/v-fib
á
Falsely elevated K
level common if:
o Hemolyzed sample (i.e. from heel stick)
o Thrombocytosis
If K significantly
elevated, repeat immediately via venous stick. Consider EKG if no set-up for
false K elevation.
HYPOKALEMIA
á If K is 3-3.5 and patient is
eating, routine diet and resolution of cause of hypo-K (i.e. DKA) are
sufficient
á If K < 3, consider supplement
with KCl: 1-2 mEq/kg/dose, goal of 2-5 mEq/kg/day
o
Liquid formulation 20 mEq/15mL
á If K <2.5, patient NPO, use IV replacement: 1 mEq/kg
dose at max rate 0.5-1 mEq/kg/hr
o
Requires continuous cardiac
monitoring!
HYPERKALEMIA
Urgent treatment of hyper-K with EKG changes: move patient to PICU if not already there
á
T- wave changes: give
1-2 mEq/kg sodium bicarb over 20 min (as D5W + 150 mEq/L sodium bicarb)
á
Widened QRS: give 20
mg/kg Calcuim chloride over 5 min
o Or 100 mg/kg calcium gluconate, but this is slower to take
effect\
o This stabilizes
the cardiac cell membrane but does not change potassium level
Mechanisms for decreasing serum K:
á
Driving K into cells:
o Sodium bicarb to increase serum pH (see above dosing)
o Insulin 0.3u/kg plus glucose 1-2g/kg
o Beta-agonists (albuterol) – can do continuous. Use if
you need to try everything.
á
Eliminate K from the
body:
o Lasix: 1 mg/kg max of 40 mg – will also eliminate H+
and Na.
o Kayexalate: 1 g/kg PO or PR
o Dialysis
HYPOCALCEMIA
Definition:
á
Total serum calcium of
< 7.0 mg/dl or ionized calcium <0.87 mmol/l.
Replacement:
á
asymptomatic patient: use oral supplements
o Calcium carbonate (TUMS, childrenÕs antacid liquid
á
Symptomatic (tetany,
hyper-reflexia, prolonged QT): use IV, slowly,
via central IV access with continuous EKG
monitoring
o Calcium Chloride (10%) 20mg/kg, max dose 1 gram
o Calcium Gluconate (10%) 50 mg/kg max dose 2 grams
á Treat hypomagnesemia – if Mg low, Ca level will not
respond well to supplements
Failure to Thrive
Definition
There is no consensus definition for FTT. Various guidelines:
á Weight for length <10%ile in child <2 years
á Weight <80% of ideal body weight
á Weight <2%ile on more than two occasions, using growth chart corrected for gestational age and any known condition (ex: Trisomy 21, achondroplasia)
á Crossing of two or more percentile lines on the weight curve over time
o Endocrine causes ˆ height drops more than or sooner than weight
o Genetic/neurologic causes ˆ small head circumference
á Rate of weight gain less than expected for age (in infants), in g/day
Etiology
á Inadequate nutrition intake
o Psychosocial
factors: eating patterns, economic difficulty, unstable environment, poor
parent/child interaction, neglect, lack of parental knowledge – most common cause. No longer a diagnosis of
exclusion.
o Poor diet: too much juice/fluids, inappropriate formula mixing
o Anatomic/physiologic problems: cleft palate, micrognathia, CP, hypotonia, weakness, GERD, Chronic constipation ˆ early satiety/poor appetite
á Inadequate absorption or increased losses
o Malabsorption: CF, celiac disease, disaccharidase deficiency, protein-losing enteropathy, IBD, milk protein allergy, parasites
o Biliary atresia
o Short bowel syndrome
o Obstruction: pyloric stenosis, malrotation
á Increased metabolic demand
o Congenital heart disease, chronic respiratory disease (CLD, OSA), CF, IBD, systemic inflammatory process (rheumatologic disease), chronic infection (TB, HIV), inborn errors of metabolism, RTA
Evaluation
á History
o PMH: detailed birth history. Gestation, birth weight, in utero exposures, newborn course, newborn screens, development, behavior issues (esp toddlers), growth charts, illnesses, hospitalizations, medications, DIET, stooling/voiding patterns. Complete ROS.
o FH: parentsÕ heights, siblings early medical history, any children in the extended family with special needs, any known medical problems in the family, any premature deaths in family
o SH/DIET: who is at home? Stable environment? Is there conflict? Is there a daily routine? Who feeds the child, feeding schedule, what types of foods are eaten. Walk through a day of feeding. Picky or not? If infant, how is the formula mixed? Amounts of water, juice, milk? Preference for drinking over eating? Grazing or set meal times? Toddler still using a bottle?
á Exam
o Observation – parent/child interaction. Activity, engagement, demeanor of child. If possible, observe a meal.
o Full physical exam including complete neuro exam. Get a head circumference.
á Lab evaluation
o First tier: CBC-d, ESR, CMP, urinalysis, pre-albumin. Lead level if high-risk and has not been done.
¤ Looking for signs of chronic disease (anemia, high ESR), malignancy (CBC), RTA, liver dysfunction (hepatitis or hepatic anomaly, IEMs).
¤ These labs are rarely diagnostic.
o Further evaluation: based on history, exam, and first-tier lab findings.
á While inpatient
o Strict I/O – give caregiver a piece of paper to write down everything the child eats or drinks.
o Nutrition consult – to evaluate nutritional needs, current diet, specific suggestions for change
Obesity and Co-morbidities
DEFINITIONS
BMI percentile for age
- Underweight: < 5th percentile
- Healthy weight: 5-84th percentile
- Overweight: 85-94th percentile
- Obese: ³ 95th percentile
¯ 95% BMI estimate after 9 years of age
¤ Boys: Age in years + 13
¤ Girls: Age in
years + 14
ETIOLOGIES
á
Exogenous: by far the
most common. Excess caloric intake.
á
Hypothyroidism
á
CushingÕs syndrome
á
Genetic syndromes:
Prader-Willi, Down Syndrome, Albright hereditary osteodystrophy, Bardet-Biedl
syndrome, Beckwith-Wiedemann
á
Medications: steroids, atypical antipsychotics
COMORBIDITIES AND SIGNS/SYMPTOMS
á
General: stature.
o Tall stature c/w exogenous obesity.
o Short stature/slow growth concerning for secondary cause of
obesity.
á
CV: Hypertension, LVH,
atherosclerotic disease, hyperlipidemia
o Headaches, chest pain, vision changes. Listen for murmur,
check BP
á
Pulmonary: Obstructive
sleep apnea
o Snoring, daytime somnolence, inattentiveness, headaches
á
GI: GERD/hiatal
hernia, gallbladder disease, fatty liver
o Heartburn, post-prandial pain, vomiting, biliary colic, RUQ
tender to palpation, hepatomegaly
á
Neuro: pseudotumor
cerebri
o Blurry vision, headaches. Examine fundi for papilledema
á
Endocrine: Insulin
resistance/type 2 diabetes, PCOS
o Polydipsia/polyuria, weight gain/loss, menstrual
irregularity/amenorrhea, acanthosis nigricans, hirsutism, acne
á
Ortho: SCFE or Blounts
disease
o Assess gait, hip/knee pain
á
Psych:
Depression/anxiety, eating disorders
á
Derm: acanthosis
nigricans (see above), candida infections, folliculitis, Hydradenitis
supprativa
o Look for striae (CushingÕs-will be violaceous), dryness and
hair loss (thyroid)
o Abscesses (particularly in groin and axillary area)
o Xanthomas
RECOMMENDED EVALUATION FOR OBESE CHILDREN
- All obese children:
- History and physical exam
- Blood pressure/pulse & growth
parameters
- Medication history
- Screen for Co-morbid diseases based on
Hx & PE
- Lipid panel (non-fasting. Only TG are affected by recent meal. If TG high, check
fasting)
- CMP
- (A1c, Vitamin D level, insulin)-not part of AAP guidelines but
could be considered
- Urine dip for
glucose and protein (if suspect for diabetes or elevated BP)
- Consider based
on history & PE:
- Obese with
poor growth: bone age.
- Sleep study
- Thyroid function tests
- LH, FSH, Free Testosterone, and 17-OHP
LABORATORY PARAMETERS
|
Prehypertension |
Systolic or diastolic BP >
90th percentile for age or 120/80, whichever
is less |
|
Stage I hypertension |
Systolic or diastolic BP
>95th percentile |
|
Stage II hypertension |
Systolic or diastolic BP
>99th percentile |
|
Impaired fasting glucose |
Glucose
100-125 mg/dL |
|
Impaired glucose tolerance |
Glucose
³140 mg/dl at one hour after 50g gtt |
|
Insulin resistance |
Insulin
³ 20 microIU/ml when fasting |
|
Diabetes Mellitus |
A1c
>6.5, random glucose >200 mg/dL with classic signs/symptoms, OR fasting
glucose >125 mg/dL |
|
Microalbuminuria |
Microalbumin : Cr ratio >30 mg/g |
LIFESTYLE COUNSELING
- B5210 every day:
¯ Eat breakfast
¯ 5 servings of fruits and vegetables (more veg than fruit)
¯ Less than 2 hours of screen time. No TV in the bedroom
¯ 1 hour of physical activity
¯ 0 sugar-sweetened beverages
- Watch portion
size: Òchoose my plateÓ is a good resource
- Avoid simple
sugars
- Adequate sleep
for age.
- Lifestyle change
for the whole family, not just the child.
COMORBID TREATMENT
LIFESTYLE MODIFICATION is the
first line of treatment for all comorbidities. In addition, if further
treatment is needed:
- Hypertriglyceridemia
¯ Decrease saturated fats and &
avoid trans fats (will need education on which foods contain these fats)-7-10%
of total calories, <300mg of cholesterol per day
¯ Increase fiber intake to age in
years + 5g, or at least 25g in adolescents
¯ If TG >600, may try omega-3
supplementation (limited data)
- Elevated LDL cholesterol
¯ Statins are approved for children
>10 years with significant dyslipidemia who have failed lifestyle
modification and have CVD risks factors. Refer to guidelines.
¯ There is no long-term safety data
in children. Statins would generally be started in consultation with a
specialist.
- Elevated A1c
¯ A1c 5.7-6.5: lifestyle modification
only
¯ A1c 6.6-8: Metformin
¤ Start at 500 mg with food. Can
increase by 500mg to max 1000 mg BID
¤ Add multivitamin daily, consider
using Metformin ER to reduce GI upset
¤ Monitor A1c q3 months, adjust
dose accordingly
¤ Monitor LFTs, Cr at baseline and annually.
¤ If A1c >6.5% consider OGTT
¯ A1c >8: initiate insulin
therapy. Refer to endocrinology.
ALTE/BRUE
Definition
BRUE (brief resolved unexplained event) has replaced the term ALTE (apparent life-threatening event). It is a sudden, brief, now resolved episode in a patient <1 year of age with no explanation for the event identified by history and physical exam, involving one or more of the following:
á Absent, decreased, or irregular breathing
á Cyanosis or pallor
á Marked change in tone (hyper- or hypotonia)
á
Altered level of responsiveness
Etiology
Etiology can be identified in about 50% of ÒALTEÓ cases, eliminating them from the BRUE definition and from the guidelines that follow. Common etiologies and suggestive history:
á GER(D) – approx 30% of ALTE dx
o Emesis at time of ALTE
o Occurred while awake and supine
o Respiratory effort but no air entry (obstructive apnea from laryngospasm due to GER)
á Seizure – approx 10-20% of ALTE dx due to CNS problems (sz, hydrocephalus, ICH)
o Loss of muscle tone during event, history of repeated ALTE
o NO history of choking/gagging
o Diagnosis made by detailed history, usually NOT by EEG (often normal)
á Respiratory infection – approx 20% of ALTE dx
o History of URI symptoms
o Specific associations: pertussis, RSV in young infants
á NAT
o Suffocation, abusive head trauma, poisoning
o See NAT section for evaluation
á Less common:
o Arrhythmia, CHD (coarctation, shunting lesions), IEM, CO intoxication, volvulus, sepsis, central hypoventilation, apnea of prematurity
Concerning historical features:
á History of sibling with SIDS or BRUE
á FH of sudden cardiac death, arrhythmia, or cardiac conduction defects
á Inconsistent hx, social concerns – concern for NAT
o Previous DSS or law enforcement involvement
á Signs/symptoms of sepsis
á More than one episode in 24 hrs
á Need for more intervention than simple stimulation
á Hx of perinatal asphyxia/hypoxic event
Concerning physical exam findings:
á Abnormal vital signs
á Irregular heart rhythm
á Bruising or signs of trauma
á
Dysmorphic features/congenital anomalies
á
Bulging fontanel/macrocephaly – concern
for bleeding
á
Abnormal tone or level of responsiveness,
abnormal pupillary exam
Evaluation
Detailed H&P. If this reveals the event to be non-life threatening and if a probable cause is identified, no further evaluation is needed. If there is concern for an underlying cause that could lead to further life-threatening events, evaluate based on your clinical judgment. If a probable cause is identified, the event is not a BRUE. The guidelines below do not apply to cases in which a cause is identified.
AAP Guidelines for BRUE, 2016
Stratification in to
risk groups:
á Lower risk: must meet all of the following criteria:
o Age >60 days
o Gestational age >/= 32 weeks, post-conception age >/= 45 weeks
o No prior BRUE, single event, not a cluster
o Duration <1 minute
o No CPR required by trained medical provider
o No concerning historical features
o No concerning physical exam findings
á Higher risk:
o Any patient who fails to meet all of the above criteria for Òlower risk.Ó
Management according
to risk group
á Higher risk:
o no evidence-based guidelines. Use clinical judgment.
á Lower risk:
o You should:
¤ Educate the family about BRUE
¤ Shared decision-making re: evaluation, disposition, follow-up
¤ Offer CPR video
o You may:
¤ Obtain EKG and pertussis testing
¤ Briefly monitor with serial exams and continuous pulse-ox
o You should not:
¤ Admit for cardio-respiratory monitoring
¤ Evaluate with blood work (CBC, CMP), viral respiratory swab, chest x-ray, echo, EEG, or upper GI
¤ Start acid suppression or anti-epileptic medication
Suggestions for management of NOT lower-risk patients (not based on AAP guidelines)
á Indications for hospitalization:
o Less than 1 month of age
o Any of the following Òred flagsÓ
¤ Signs/symptoms of sepsis
¤ More than one event in 24 hrs
¤ History of sibling with SIDS or FH of sudden death
¤ Bruising or signs of trauma, other concern for NAT
¤ Dysmorphic features or congenital anomalies
¤ Need for significant stimulation to return to baseline
á Goals of hospitalization:
o Observing any episodes- may lead to diagnosis or indicate further work-up
o Observing parent/child interaction and feeding – guides appropriate anticipatory guidance
o Reassurance for the family
á Tests that are NOT usually helpful:
o EEG – often normal even if seizure was the cause of the event
o Upper GI – will usually show GER, but cannot determine if this is pathologic
o Sleep study – most often normal even if the event occurred during sleep
á Tests that may help in specific situations:
o Swallow evaluation – bedside or video. If micrognathia, malformations, history of poor feeding and feeding-associated event
o CMP – if concern for IEM.
o UDS – if altered sensorium
o EKG – especially if FHx of arrhythmia, sudden death at a young age
o NAT evaluation if suspected: skeletal survey, head imaging, funduscopic exam, LFTs
Physical Abuse
Epidemiology: Anyone, any family, any sex for victim or perpetrator.
Risk Factors: Stress in the parent or child or family
When
to suspect:
á Injury (bruise, burn, facture, head injury) is not plausible with patientÕs development
á History changes over time or between caretakers
á Excessive delay in seeking medical care
History
**
History is taken from parent alone, not in childÕs presence **
á Document history as it is told to you (do not summarize or rearrange the story)
á Keep asking questions until you can picture exactly what happened
Examination
á Complete physical examination (you have to see it all)
á Document everything you see (clear descriptions, a picture with words)
Evaluation/Management
**for all types of physical abuse: bruises, fractures, burns,
AHT**
1) Consult Child Abuse (day or night)
2) Consult Social Work to assist in reporting to DSS and Law Enforcement
3) Child < 1 year of age Head CT (not an ultrasound, you will miss posterior fossa)
4) Child < 2 years of age Skeletal Survey
5) If intracranial injury, Consult ophthalmology
6) If abdominal injury suspected (ie injury to torso), CMP, amylase, lipase
a. Abdominal and Pelvic CT if labs elevated
b. (AST, ALT >80, any elevation in amylase or lipase)
Footnote:
Call Child Abuse with any questions
day (898-1470) or night (on call center)
Sexual Abuse
Epidemiology: Anyone, any family, any sex for victim or perpetrator
When
to suspect:
á Parent reports that the child gave a disclosure (most common)
á Child has an STI (including herpes and warts)
á Sibling of a sexual abuse victim
Last
contact with Perpetrator
**
History is taken from parent alone, not in childÕs presence **
Less than 72 hours
1) Activate SANE Protocol
2) Consult Social Work to assist in making a report to DSS and Law enforcement
Greater than 72 hours or unknown
1) Examine child for any obvious injuries (including genital examination)
2) Consult Social Work to assist in making a report to DSS
3) Referral to ARC
Footnote:
Call Child Abuse with any questions
day (898-1470) or night (on call center)
General Approach to Poisonings/Ingestions
CLINICAL SUSPICION
á
Altered consciousness,
seizure activity or unusual behavior. Ingestion often unwitnessed.
á
Toddler age
(unintentional) or adolescent (intentional) most common ages.
á
Major toxicities:
o CV: arrhythmia, prolonged QRS or QT
o Metabolic: metabolic acidosis, hypoglycemia
o CNS: coma, seizure, AMS, hallucination
o GI: abdominal pain, vomiting, diarrhea.
STEPS IN EMERGENCY
MANAGEMENT
- ABCs! Stabilize
first.
¯ In suspected ingestion, stat EKG & POC Glucose in ill-appearing patient
- Decontamination
measures to remove further hazards:
¯ chemicals on the patientÕs clothing and/or skin
¯ flushing eyes as appropriate
- History:
¯ what, when, how much ingested
¯ treatments attempted at home
¯ pertinent past medical history (ex: current meds, cardiac hx,
epilepsy)
- Exam:
¯ Vitals, pupils, mental status, CV exam, perfusion, skin
¯ Look for findings c/w specific toxidrome or non-ingestion
cause of symptoms
- Labs for any
suspected ingestion:
¯ BMP/CMP +/- serum osm, UDS, EKG, Tylenol, salicylate, and
ETOH levels
- Consider based
on presentation:
¯ Head CT, specific drug levels (known home med OD)
¯ Abdominal imaging (concern for iron ingestion)
- Call poison control:
1-800-222-1222
¯ Once ingested substance is known
¯ If ingested substance unknown, call to discuss w/u and
intervention
GI DECONTAMINATION
á
Activated charcoal (0.5-1 g/kg, max of 50g, one dose only)
o Use
indicated if presentation is within 60 minutes of
ingestion to prevent further absorption in alert patient
¤ Little evidence for efficacy.
¤ Can be beneficial in Ôdelayed releaseÕ ingestions
o Multi-dose
activated charcoal may be useful for life-threatening
overdoses of:
¤ phenobarbital, tegretol, theophylline, dapsone, quinine
o CAN decrease absorption of some additional medications.
¤ Phenytoin, TCAs, digoxin
o CANNOT use for:
¤ heavy metals, lithium, alcohols, solvents, hydrocarbons,
cyanide, caustics
o Contra-indications:
¤ AMS, risk of aspiration, intestinal obstruction, ileus
(relative)
o Adverse effects:
¤ Aspiration pneumonia, constipation, vomiting, abdominal pain
á
Whole Bowel Irrigation: rarely used. Considered if large amount of enteric-coated or
delayed-release medication ingested. Use only in consultation with
toxicologist.
OTHER DECONTAMINATION
METHODS
- Hemodialysis:
- Indicated for
extreme toxicity with aspirin, lithium, phenobarbital, theophylline, and
alcohols
á Urine alkalinization
o Use for elimination of weak acids like salicylates,
barbiturates, methotrexate
o Use sodium bicarbonate by bolus (1 to 2 mEq/kg) or
continuous infusion (D5W with 150 mEq/L NaHCO3 at 1.5-2x maintenance
rate)
o Goal urine pH of 7 to 8
o
Must monitor serum
electrolytes
COMMON INGESTED
SUBSTANCES - MANAGEMENT
- Acetaminophen:
The most common pediatric ingestion
- Toxic dose:
>150 mg/kg in a child or 7.5 g in an adult patient
- Pathogenesis:
metabolized to NAPQI which is conjugated by GSH ˆ
GSH depleted ˆ oxidation damage to
liver by NAPQI ˆ liver failure
- LFTs
rise at 24-48 hrs, peak at 72-96 hrs
- Check acetaminophen level at 4 hrs,
or ASAP if later presentation
- Plot
on Rumack-Matthew nomogram to determine need for treatment
- Repeat
level at 8hrs if extended-release tabs ingested
- Antidote:
N-acetylcysteine
- 150
mg/kg over 1 hr (max 15g), then
- 50mg/kg
over 4 hrs (max 5g), then
- 100
mg/kg over 16 hrs (max 10g)
- Salicylates
include: aspirin, bismuth
subsalicylate (pepto-bismol), methyl salicylate (wintergreen oil)
- Toxic dose:
> 150 mg/kg
- Therapeutic
level 10-30 mg/dL, toxic above 30-50 mg/dL
- Level
>100 mg/dL = indication for dialysis
- Pathogenesis:
uncouples oxidative phosphorylation ˆ
hyperthermia. Triggers central hyperventilation ˆ
respiratory alkalosis. Causes high AG metabolic acidosis, hypoglycemia, hypokalemia
- Symptoms:
nausea/vomiting; tinnitus; altered mental status, tachypnea, pulmonary
edema, coma
- Management:
- ABCs.
- IVF
with dextrose and bicarb to alkalinize (enhances renal excretion)
- Follow
urine pH, goal >7.5
- Replete
potassium if low (low K ˆ acidic urine)
- Interpretation of salicylate level must be made in conjunction with serum pH. (i.e. more acidosis = more severe toxicity regardless of serum ASA level)
- Follow
salicylate level Q2h until falling x2
- Follow
blood gas Q2h until pH stable x2 (goal 7.45-7.5)
- Clonidine
- Pathogenesis:
alpha-2 agonist. At very high dose, some alpha-1
- Symptoms:
hypotension, bradycardia, miosis, depressed consciousness, respiratory
depression
- Large
ingestion can lead to initial paradoxical HIGH BP that then drops to
hypotension as drug is metabolized (due to initial alpha-1 activity)
- Onset
30-90min, duration up to 3 days
- Supportive
care for BP, respiratory status with telemetry monitoring.
- Naloxone 0.1mg/kg may
have potential to reverse some symptoms.
- Tricyclic
Antidepressants
- Pathogenesis:
decrease re-uptake of nor-epi, Ach, serotonin. Also blocks H1 receptors,
affects dopamine, alpha-1 receptors
- Signs/Symptoms:
rapid onset AMS indicates
significant ingestion
- Anticholinergic:
hot dry skin, miosis, AMS, urinary retention, tachycardia
- CV:
sinus tachy, heart block, prolonged QTc, wide QRS ˆ v-tach, v-fib, hypotension
- CNS:
AMS, coma, seizure
- Treatment:
- Supportive.
ABCs, benzos to stop seizure or for agitation
- If
arrhythmia or hypotension: 1-2 mEq/kg sodium bicarbonate bolus
- Then
bicarb fluids to maintain pH 7.5
- Opioids
- Symptoms: CNS
depression, respiratory depression, bradycardia, miosis, constipation,
urinary retention
- Synthetic
opioids (all but morphine, codeine) do not always cause positive UDS
- Evaluation: 1st
tier above + blood gas.
- Treatment:
- Supportive
care: ABCs. May require ventilation, BP support.
- Naloxone:
for respiratory depression.
- 0.1
mg/kg to max of 2 mg Q 3-5 min until improvement in resp status. If no improvement after 5 doses,
stop.
- If
opioid dependence suspected, use 0.4 mg Q3-5 min. Full dose could
provoke withdrawal seizure.
- Short-acting.
May need repeat dosing or continuous infusion if long-acting drug
ingested.
- Toxic
Alcohols: ethanol, isopropanol,
methanol, ethylene glycol
- Common
household chemicals: antifreeze, rubbing alcohol, liquor, paint, varnish
- Signs/symptoms/toxicity:
CNS depression
- Methanol:
metabolized to formate ˆ retinal injury,
CNS hemorrhage (basal ganglia). Elevated AG acidosis
- Ethylene
glycol: metabolized to oxalate ˆ
crystals in kidney ˆ AKI, slower
elimination. Elevated AG acidosis
- Isopropanol:
CNS depression, resp depression, low BP, no acidosis
- Ethanol:
CNS depression, resp depression, may
have acidosis with normal AG but will have osmolar gap
- Management:
- For
methanol, ethylene glycol: fomepizole. Blocks alcohol dehydrogenase ˆ prevents formation of toxic metabolites
(formate, oxalate)
- For
all: ABCs, fluids, normalize pH, supportive care
Inborn Errors of Metabolism and Metabolic Diseases
COMMON SIGNS AND SYMPTOMS
- Symptoms
of lethargy, poor feeding, vomiting, apnea, tachypnea
- Acute
encephalopathy or seizures
- Unexplained
jaundice, liver failure, metabolic acidosis, or hypoglycemia
- Dysmorphic
features or unusual odors
- Myopathy
- Failure
to thrive
MOST are autosomal recessive and present in neonates or young children.
IEM PRESENTATIONS AND ASSOCIATED DISORDERS
|
Class of Disorders |
Characteristic Lab
Findings |
|
Organic Acidemias (includes
Methylmalonic acidemia, Proprionic acidemia, Isovaleric acidemia) |
á Metabolic acidosis with increased AG á + Plasma and urine ketones á Elevated plasma ammonia and lactate á Abnormal urine organic acids á Low WBC, plts can be present |
|
Urea Cycle Defects (includes
Ornithine transcarbamylase deficiency, Citrullinemia) |
á VERY elevated plasma ammonia á No metabolic acidosis á No ketonuria á Variable respiratory alkalosis á Elevated orotic acid in OTCD á Abnormal plasma amino acids |
|
Fatty Acid Oxidation (includes Medium chain acyl-CoA dehydrogenase deficiency) |
á Nonketotic hypoglycemia with illness, stress, prolonged fast á Metabolic acidosis, hyperammonemia á Elevated acylcarnitine á Presents when infant feedings spaced out |
|
Amino acidopathies (includes
PKU, Maple Syrup disease, Homocystinuria) |
á Metabolic acidosis with increased AG á Elevated plasma amino acids |
|
Glycogen Storage
Diseases |
á Fasting ketotic hypoglycemia á +/-hepatomegaly á Symptoms worse with fasting |
|
Mitochondrial
Disorders (includes MELAS, Pyruvate dehydrogenase deficiency, Pyruvate
carboxylase deficiency) |
á Elevated lactate and pyruvate á Wide variety of presentations |
|
Nonketotic
Hyperglycinemia |
á Acute encephalopathy á No metabolic acidosis á No hyperammonemia á Abnormal plasma amino acids |
LABORATORY EVALUATION FOR IEM
If possible, laboratory evaluation should be obtained while
the patient is symptomatic, because metabolites of certain disorders are not
detectable when the patient is asymptomatic.
First Tier Evaluation
- ABG for pH
- CMP- calculate anion gap
- CBC
- Ammonia
- Urinalysis
- Urine and plasma amino acids
- Urine organic acids
- Urine reducing substances
- Plasma lactate and pyruvate
- If hypoglycemic, obtain critical sample (see ÒHypoglycemiaÓ section)
Second Tier Evaluation
- Guided by clinical suspicion and first-tier findings.
MITOCHONDRIAL DEFECTS
Consider when complex neurological or multisystem involvement is present. Virtually any organ system or presentation is possible. Can present in infancy or at any age, sometimes triggered by a stressor such as acute illness. All disorders of mitochondrial DNA are maternally derived.
PRESENTATIONS OF MITOCHONDRIAL DEFECTS
|
Organ System |
Possible Involvement |
|
Central Nervous System |
Encephalopathy, mental
retardation, ataxia, strokes, deafness, seizures |
|
Cardiovascular |
Cardiomyopathy, heart block |
|
Gastrointestinal |
Liver disease, pancreatic
insufficiency, villous atrophy, poor GI motility |
|
Endocrine |
DM, DI, hypoglycemia |
|
Musculoskeletal |
Myopathy |
|
Renal |
Renal tubular acidosis |
|
Heme |
Pancytopenia, neutropenia,
or anemia |
EMERGENT THERAPY FOR POSSIBLE IEM
á Goals:
o Prevent further accumulation of toxic metabolite
¤ Send diagnostic labs, make NPO, give IV dextrose for energy source to prevent catabolism
o Eliminate toxic metabolite from body: diagnosis-specific
¤ Urea cycle disorders: arginine
¤ Elevated ammonia: Ammonul (sodium phenylacetate + sodium benzoate), may need dialysis
¤
If
patient with known diagnosis, ask family about the Òsick dayÓ plan
*THAN-Transient Hyperammonemia of Newborn
Kawasaki Disease
Kawasaki Disease (KD) is an acute febrile, systemic vasculitis of unknown etiology. If untreated, it can result in coronary artery abnormalities in up to 25% of cases. The diagnosis of KD is based on clinical criteria as established by the CDC.
EPIDEMIOLOGY
á Most common in ages 1-4
á Rare in older children and in infants <6 months
á Patients at higher risk for coronary artery aneurysms:
o Infants
o African American
o Boys
DIFFERENTIAL DIAGNOSIS
- Toxin mediated illness: scarlet fever, toxic shock syndrome, staph scalded skin
- Stevens-Johnson syndrome/drug reactions
- Collagen vascular disease - JIA
- Rheumatic fever
- Subacute bacterial endocarditis
- Serum sickness
- RMSF/other rickettsial disease, leptospirosis
- Viral syndromes: EBV, Hepatitis B, adenovirus, influenza, measles
DIAGNOSIS
Diagnosis is based on exclusion of other etiologies and the fulfillment of clinical criteria. Requires 5+ days of fever and 4/5 of the following criteria. Patients are classically very irritable.
|
|
|
|
Criteria |
Comments |
|
Bilateral non-exudative conjunctivitis |
|
|
Polymorphous exanthem |
|
|
Cervical lymphadenopathy |
|
|
Changes in the hands or feet |
|
|
Changes of the oropharynx |
|
|
Associated Features – NOT part of
diagnostic criteria |
|
|
Clinical Findings |
Laboratory Findings |
|
|
INCOMPLETE KAWASAKI DISEASE
- Some
patients do not fulfill the above criteria and are subsequently diagnosed
with ÒincompleteÓ or ÒatypicalÓ Kawasaki Disease
- Incomplete
KD is more common in young infants.
- Evaluation
of suspected incomplete Kawasaki disease includes the following
Òsupplementary lab criteriaÓ
- Anemia
for age
- Plts
>450K after day 7
- WBC
>15,000
- Albumin
<3
- ALT
>70
- Sterile
pyuria (>10 WBC on UA)
- For
the diagnostic algorithm below, also need CRP, ESR
- Infants
² 6 months old on day ³ 7 of fever without other explanation, even
if no clinical features of Kawasaki, should have laboratory testing:
- CBC,
ESR, CRP, CMP, UA
- If
evidence of systemic inflammation, need echo
- See
algorithm for workup of children with suspected incomplete KD
CARDIAC INVOLVEMENT
á Classic cardiac involvement is coronary artery aneurysm – can occur at any time in acute or subacute phase of illness
o It is the main cause of morbidity and mortality
á Other cardiac findings can include:
o Pericardial effusion, LV dysfunction, mitral regurgitation
MANAGEMENT AND THERAPY
- Echocardiogram should be performed at time of diagnosis and repeated 6-8 weeks later
- If no coronary abnormalities or initial coronary artery ectasia that has resolved by 6-8 weeks, no long-term medications or activity restrictions needed
- If coronary artery abnormalities at 6-8 weeks, need to be followed by cardiology and most often require long-term low-dose aspirin
- IVIG 2 g/kg should be given when diagnosis is made.
- Goal timing is on days 5-9 of fever
- Treatment before day 5 has higher risk of relapse and need for repeat treatment
- Treatment after day 10 does resolve inflammation but does NOT decrease risk of coronary artery aneurysm, which is the major goal of treatment
- See appendix for IVIG protocol and
adverse reactions
- Aspirin 30-50 mg/kg/day divided TID-QID (Òmedium doseÓ) until afebrile x48 hr
- For anti-platelet and anti-inflammatory effect
- Decrease to 3-5 mg/kg when afebrile x48 hrs (Òlow doseÓ)
- Continue low-dose aspirin until inflammatory markers and platelets normalize
- Patients with coronary artery aneurysms require prolonged low-dose aspirin
- Monitor ESR, platelets weekly until normal – to know when to d/c aspirin
- Failure to respond:
- If persistent fever 48 hrs after IVIG, repeat dose
- If still febrile 48 hrs after second dose of IVIG, repeat dose and add steroids
- Methylprednisolone 30 mg/kg/day divided BID for 3 days
- Live virus vaccines should be delayed
11 months after receiving IVIG to avoid suppression of immunologic
response to the vaccine
Radiologic Studies and Basic Indications
This is NOT an exhaustive list!
Head Imaging
á Head ultrasound – screening
imaging study in infants <6 months
o
Can detect bleed, hydrocephalus, tumor depending
on location.
¤ Not adequate for suspected
traumatic bleed (NAT or accidental)
o
Does not image the periphery of the brain or posterior fossa well.
Dependent on fontanel size.
o
Normal study despite clinical suspicion ˆ order further imaging
á CT – without contrast to
r/o acute bleed, skull fx, herniation/increased ICP
o
Use in significant head trauma, esp w/ LOC, depressed GCS, clinical sign
of fx
¤ Also image c-spine unless clear
evidence spine is ok
o
May use prior to LP if too urgent to wait for MRI
á MRI
o
Without and with contrast
¤ Tumor, abscess,
meningitis/encephalitis, MS, ADEM, new onset seizure, vascular malformation,
developmental delay, eval of pituitary
o
Without contrast
¤ To evaluate anatomy, headache,
trauma, NAT (shaken baby)
o
MRA –for AVMs, moya moya, consider if concern
for ischemic stroke (sickle cell!)
o
MRV –for venous sinus thrombosis, LemierreÕs disease
GI Imaging
á Ultrasound – Numerous
indications. imaging of choice for:
o
Female pelvis: ovarian torsion/cyst, pregnancy, most pelvic pathology
o
Male: testicular torsion, testicular mass
o
Hydronephrosis/cystic kidney disease
o
Initial eval of liver, spleen without radiation of a CT
o
US of pylorus for hypertrophic pyloric stenosis
o
First imaging ordered to evaluate for appendicitis. If inconclusive, then
CT
o
*quality can be limited by body habitus, bowel gas,
operator skill
á X-ray
o
Flat plate –assess stool burden, ingested FB. If exam concerning,
do flat+upright.
o
Flat and upright/lateral decubitus – concern for obstruction or
perforation (air-fluid levels, free air)
á CT scan – always order WITH
contrast
o
Numerous indications, generally in more severe illness
o
Evaluation of the acute abdomen
á Upper GI
o
Upper GI only – follows contrast through duodenal c-loop. Mainly
for anatomical abnormalities.
¤ Imaging study of choice for
malrotation. 95% sensitivity.
¤ Will commonly show reflux in
young infants. Cannot distinguish physiologic from pathologic. Indication in an
infant with severely symptomatic reflux is to look for anatomic abnormality
(i.e. hiatal hernia)
¤ Will show external compression
from vascular ring/sling
o
UGI w/ small bowel follow-through
¤ If concern for
malrotation/obstruction more distal than duodenum.
¤ Can show signs of IBD (i.e. string sign, fistulas, narrow
lumen w/ nodularity) but is not imaging of choice
á Esophagram
o
Shows only esophagus. Can show TEF (if done with pressure), stricture,
web, compression from ring/sling
á Water-soluble contrast enema
o
Diagnostic and therapeutic in severe constipation but VERY expensive
¤ Use when large distal stool
burden not responsive to regular enema
o
Chronic constipation: eval anatomy for HirschsprungÕs, megacolon
¤ Evaluating for HirschsprungÕs: no
bowel prep or rectal stim for 24h prior to procedure
á Air contrast enema (barium)
o
Diagnostic and therapeutic for intussusception
o
Notify surgeon before enema is done. Risk of perforation requiring
surgery.
Hepatic/Biliary Imaging
á Ultrasound
o
Excellent for gallbladder pathology: gallstones, obstruction, inflammation
o
Screening exam for biliary atresia. Must be NPO 8 hrs to distend
gallbladder
á HIDA scan: nuclear medicine scan
to evaluate bile drainage. Use to evaluate for:
o
Biliary atresia
o
Cholecystitis
o
Biliary dyskinesia
á MRCP: for further delineation of anatomy seen
with other imaging modalities
Chest Imaging
á X-ray
o
Many indications
o
NOT indicated in diagnosis of: asthma, bronchiolitis, neonate with fever
but no respiratory symptoms
á Ultrasound
o
Pleural effusion v. empyema: most sensitive for dx of loculations
o
Increasing use as primary imaging rather than CXR in dx of pneumonia
á CT
o
Eval after trauma with severe
chest injury
o
Eval of bronchiectasis or persistent infiltrate
o
Further eval of large effusion or abscess seen on x-ray or US pre-op
o
Eval for metastatic disease or mediastinal mass
o
Concern for foreign body with inconclusive x-rays
o
NOT commonly used in general hospital pediatrics
Pediatric Nutrition - Formulas
Term Infant Feeding
**unless otherwise noted, measure 2 oz water, add 1 level, unpacked scoop of powder to prepare.
á Breastmilk: preferred source of nutrition. 20 kcal/oz
á Basic formulas: 20 kcal/oz, minimal differences in content.
o Good Start Gentle
o Similac Advance (19 kcal)
o Enfamil Lipil
á Basic formulas with special marketing for ÒcolicÓ or gas. 20 kcal/oz
o Good Start Soothe – has probiotic, 30% lactose, partially hydrolyzed protein
o GoodStart Extensive HA – 100% whey protein, some MCT, partially hydrolyzed protein
o Similac Sensitive (19 kcal) – reduced lactose
o Similac Total Comfort (19 kcal) – partially hydrolyzed protein
o Enfamil Gentlease – 25% reduced lactose
á Basic formulas with special marketing for reflux: with added rice cereal. 20 kcal/oz
o Enfamil AR
o Similac for spit-up (19 kcal)
á Soy protein-based formulas: indications = galactosemia, sometimes in milk protein intolerance (high cross-reactivity). 20 kcal/oz
o Enfamil Prosobee
o Similac Soy Isomil (19 kcal)
o GoodStart Soy
á Casein hydrolysate formulas: for milk protein intolerance. 20 kcal/oz. MCT requires no bile acid to absorb – used for pts with malabsorption, biliary disease
o Enfamil Nutramigen (no MCT) – sucrose/lactose free
o Similac Alimentum (33% MCT) – lactose free
o Enfamil Pregestimil (55% MCT) – sucrose/lactose free
á Whey hydrolysate formula: for milk protein intolerance. 20 kcal/oz, MCT requires no bile acid to absorb-used for pts with malabsorption, biliary disease
o Good Start Extensive HA (49% MCT) – 100% whey protein (mixing: 1 oz water +1 scoop powder)
á Elemental formulas: single amino acids. 20 kcal/oz. fructose, lactose, galactose-free. 33% MCT.
o Neocate – mix 1 scoop to 1 oz water
o Elecare
o Alfamino Infant (43% MCT) – mix 1scoop to 1 oz water
á Renal formula:
o Similac PM 60/40 – low phosphorus, low iron. 60:40 is ratio of whey to casein.
o **the lowest phosphorus ÒformulaÓ available is breast milk!
Pre-Term Infant Feeding
á Basic pre-term formulas: 22 kcal/oz, extra calcium, vitamins. For catch-up growth and prevention of osteopenia of prematurity. Can use until 1 yr or change to standard formula at 6-9 months if baby is gaining too much.
o Similac Neosure
o Enfamil Enfacare
Recipes for Concentrating Formula
á Breast Milk 22 kcal/oz
o 3 oz breast milk + ½ tsp standard formula powder
á Good Start 22 kcal/oz
o 3 ½ oz water + 2 scoops powder
á Good Start 24 kcal/oz
o 6 ½ oz water + 4 scoops powder
á Neosure 24 kcal/oz
o 5 ½ oz water + 3 scoops powder
á Neosure 27 kcal/oz
o 8 oz water + 5 scoops powder
Formula for Children Over 1 Year
**1.0 indicates 30 kcal/oz = 1kcal/cc, 1.5 = 45 kcal/oz, 2.0 = 60
kcal/oz
Unless otherwise specified, formulas are 30 kcal/oz
Many come in flavors for kids who take them PO
á Basic formulas (many have Òwith fiberÓ option - increase total daily water by 25% with these. Fiber is used if patient has chronic diarrhea, not constipation
o Pediasure 1.0, 1.5
o Nutren Jr – 50% whey protein, 20% MCT
o Boost Kids Essentials 1.0, 1.5
á Hydrolyzed Protein formulas
o Peptamen Jr 1.0, 1.5
o Pediasure Peptide 1.0, 1.5
á Elemental formulas
o Neocate Jr
o Elecare Jr
o Alfamino Jr
á Fat-Modified formula
o Portagen – 87% MCT. For Malabsorption and biliary disease.
Formulas for Children Over 6 Years
á Nutren 1.0, 1.5, 2.0
o 1.5, 2.0 used for patients who need fluid restriction or very high calorie diet (CF)
Formula Additives/Dietary Supplements
á Duocal
o Protein-free powder. Supplement for pts with protein metabolism problems
o 25 kcal/scoop. 59% carb/41% fat, has some MCT
á Microlipid
o Safflower oil emulsion in water. 4.5 kcal/mL, 100% fat
o To supplement calories in specialized diet, especially ketogenic
á MCT oil
o 100% fat, 7.7 kcal/mL
o Does not require bile salts to digest – used in malabsorption and biliary disease
á Liquigen
o MCT oil (Palm kernel and/or coconut oil) emulsion in water, 4.5 kcal/mL, 100% fat
o Does not reuire bile salts to digest, ketogenic, chylothorax, long chain fatty acid oxidation disorders
á Beneprotein
o 100% protein: whey protein isolate, a milk product
o 25 kcal/scoop, 6 g pro/scoop
á Salt packets
o Used for NaCl replacement in pts on diuretics
o 1 packet = 1/8 tsp = 12.8 mEq sodium
This is not an exhaustive list of available products!
Infectious Disease
Antibiotics
A brief overview of classes, common regimens
Beta-lactams: interfere with bacterial cell wall synthesis. Bactericidal.
á
Penicillins
o Penicillin: gram +, some gram (-) anaerobic coverage
¤ NOT: Neisseria, bacteroides
o Anti-staphylococcal penicillins: traditional abx of choice for MSSA. Poor gram(-) coverage. Caustic to veins, require q6hr dosing
¤ Nafcillin, Oxacillin, Dicloxacillin
o Broad spectrum penicillins: amoxicillin, ampicillin = almost identical
¤ Better gram (-) coverage
¤ Susceptible to beta-lactamases – to combat this, beta lactamase-inhibitor added: clavulic acid or sulbactam
á Amox/clav = augmentin
á Amp/sulbactam = unasym
o Anti-pseudomonal penicillins: piperacillin
¤ Strong gram (-) coverage, less gram +. Available only with beta lactamase-inhibitor:
á Piperacillin/tazobactam = Zosyn
á
Cephalosporins
o 1st gen: Cefazolin (Ancef) = IV; cephalexin (Keflex) = PO.
¤ Gram + coverage, GNR coverage (not Neisseria or H flu)
¤ Drug of choice for sensitive MSSA
o 2nd gen: cefuroxime (Ceftin, Zinacef), cefoxitin
¤ Less gram + coverage, better GNR coverage, esp against H. flu
¤ Cefoxitin has acceptable gram (-) and anaerobic coverage for simple intra-abdominal infections (see guidelines)
o 3rd gen: ceftriaxone (Rocephin) = IV/IM, cefotaxime (Claforan) = IV, cefdinir (Omnicef )= PO
¤ Broad gram + and gram (-) coverage but does not cover pseudomonas.
¤ Omnicef has poor lung penetration. Not good for PNA!
¤ Ceftazidime (Fortaz) = the only 3rd gen ceph. that covers pseudomonas!
o 4th gen: cefepime (Maxipime)
¤ Broad gram (-) coverage including pseudomonas
o 5th gen: ceftaroline
¤ Spectrum of 3rd generation + covers MRSA. No pseudomonas coverage!
o New, as yet unclassified:
Ceftolazane/tazobactam (Zerbaxa)
¤ keeps integrity with ESBL, KPC, other resistant organisms. Restricted use – possibly in CF patients
á
Carbapenems
o Meropenem (Merrem), Imipenem, Ertapenem
o VERY broad spectrum! Gram+, gram (-), anaerobe
o Use only if there is no other, narrower-spectrum option. Do not use empirically.
¤ Most often used in pt with hx of resistant organisms, based on past culture
Macrolides: azithromycin (Zithromax), erythromycin, clarithromycin (Biaxin)
á Inhibit protein synthesis by binding ribosome (reversibly) – bacteriostatic.
á Broad spectrum. Used most often for atypical infections: mycoplasma, ureaplasma, non-tuberculous mycobacteria and pertussis
o Good gram + and gram (-) coverage as well
á **adverse effects: prolonged QT interval!!
o Erythromycin linked to pyloric stenosis; also used as a prokinetic
Aminoglycosides: gentamicin, tobramycin, amikacin, streptomycin, neomycin
á Inhibit protein synthesis irreversibly: bactericidal.
á Spectrum: best against aerobic gram (-). Does cover pseudomonas but cannot use as monotherapy
o Synergistic with ampicillin
á Uses: CF exacerbations (pseudomonas, often); neonatal meningitis; part of empiric regimen for VP shunt infection
á Adverse effects: nephrotoxicity, hearing loss
Fluoroquinolones: ciprofloxacin (Cipro), levofloxacin (Levaquin), moxifloxacin (Avelox)
á Inhibit DNA gyrase to prevent cell replication. Bactericidal.
á Spectrum: best for gram (-). The only PO drugs that cover pseudomonas.
á Use: sparingly. For pseudomonas (often in CF), if no other narrower-spectrum option. Do not use empirically.
o Can use as a PO option to finish course for CAP that failed amp/amox
á Adverse effects: arthropathy, achilles tendon rupture in children is reported. GI upset common.
Other
á
Vancomycin
o Inhibits cell wall synthesis. Bactericidal
o Spectrum: gram + including MRSA
o Use: MRSA bacteremia, MRSA resistant to clindamycin, PCN-resistant s. pneumo
o Empiric coverage of: VP shunt infection, osteomyelitis, septic arthritis
á Clindamycin (Cleocin)
o Inhibits protein synthesis at ribosome. Either bacteriostatic or bactericidal.
o Spectrum: Gram +, anaerobes above the diaphragm. NOT intra-abdominal
o Use: skin and soft tissue infxn, MRSA infxn (NOT bloodstream), lymphadenitis, eradication of GABHS carrier state, oral infections
á TMP-SMX (Septra, Bactrim, co-trimoxazole)
o Inhibits folate metabolism. Bacteriostatic.
o Spectrum: Gram + (including MRSA), gram (-), NOT pseudomonas
¤ Also p. jiroveci (PCP), some protozoa
o Use: MRSA infection, UTI (empiric for GNRs or specific pathogen), PCP ppx in immunocompromised (chemotherapy, HIV)
o Adverse effect: GI upset, Stevens-Johnson syndrome
á Linezolid (Zyvox)
o Inhibits protein synthesis at ribosome. Bactericidal against strep, bacteriostatic against staph, enterococcus.
o Use: MRSA, VRE – only if there is no other narrower-spectrum option!
¤ NOT for bacteremia
o Adverse effects: agranulocysosis, bone marrow suppression
á Tetracyclines: tetracycline, doxycycline, minocycline (Minocin), tigecycline (Tygacil)
o Inhibits protein synthesis reversibly. Bacteriostatic.
o Spectrum: broad gram+, gram (-), atypical organisms
o Use: tick-borne illness, atypical infections, MRSA (if susceptibility proven), acne
¤ Ònot recommendedÓ under 8 years, but still the treatment of choice for tick-borne illness (RMSF, Ehrlichia) in children of any age
o Adverse reactions: photosensitivity, teeth staining (<8 yr old, theoretical)
á Metronidazole (Flagyl)
o Unclear mechanism. Considered bactericidal.
o Spectrum: anaerobes, protozoa
o Use: C. difficile, intra-abdominal infection, trichomonas, BV, protozoa (Giardia)
o Adverse effects: GI upset most common
Antibiotics for specific pathogens:
á Antibiotics that cover pseudomonas:
o Fluoroquinolones (the only PO option): levofloxacin, ciprofloxacin
o Pencillins: piperacillin/tazobactam
o Cephalosporins: ceftazidime (3rd gen), cefepime (4th gen), ceftolazane/tazobactam
o Carbapenems: meropenem, imipenem (NOT ertapenem)
o Aminoglycosides: do not use as single
coverage, only as adjunct!
á Antibiotics that cover MRSA:
o Ceftaroline (5th gen cephalosporin)
o Vancomycin
o Clindamycin
o TMP-SMX
o Other: tetracyclines, daptomycin, linezolid
Infant with fever of uncertain source
Guidelines for management of
infants <30 days and 30-60 days are changing based on new evidence in the
era of good vaccine coverage.
Fever: Rectal temp of 100.4 or greater (documented at home
or in a clinical setting)
RISK FACTORS FOR BACTERIAL INFECTION
- History of
prematurity
- Perinatal
antibiotics
- History of
previous rehospitalization
- Chronic illness
- Mother with
intrapartum fever, Group B Strep, or intrapartum antibiotics
RISK FACTORS FOR HSV
INFECTIONS IN INFANTS
- Ill appearance
(especially in the first 28 days of life)
- Primary maternal
HSV infection at delivery or history of HSV
- 30-80% of neonates with HSV have
mothers with NO known history of HSV!
- Known exposure
to HSV infected persons (includes cold sores)
- Fetal scalp electrodes
- Maternal history
of STDs or unexplained fever at delivery
- CSF pleocytosis
with a negative gram stain
- Failure of fever
to abate within 24-48 hrs after starting antibiotics
- Unexplained CNS
signs – such as a seizure
- Half of HSV
infected infants donÕt have fever and may present with respiratory sx
SYMPTOMS AND SIGNS
- Evident bacterial infection: treat
accordingly
- Cellulitis,
omphalitis, septic arthritis, osteo, bacterial pneumonia
- Depending on
age, severity of illness, clinical appearance, consider LP before
antibiotics
á
Symptoms
- Bronchiolitis
– treat as bronchiolitis
- URI –
Follow the pathway
- Diarrhea
– obtain stool culture and follow the pathway
- Otitis media
– follow the pathway (risk of invasive disease same as w/o OM)
PATHWAY FOR INFANTS 7-28 [MG1] DAYS
á
If documented
temperature of >100.4 at home or in ED/clinic and no source, evaluate with:
o Urinalysis by any method, and if positive a cath gram stain
and urine culture
¤ ÒpositiveÓ = LE present OR >4WBC
o Blood cultures x2
o Procalcitonin or CRP or WBC with differential
¤ *IF decision has
been made to treat with antibiotics, no need to obtain inflammatory marker.
¤ High risk criteria:
á
WBC <5,000 or
>15,000
á
Total bands >1500
o CSF culture, routine CSF studies
o If concern for HSV, send HSV PCR on blood and CSF
á
Once all cultures
obtained, decide treatment course:
o If any test abnormal (UA w/ +LE, hi-risk WBC, high CRP or
PCT, or CSF suggestive of bacteria, start empiric antibiotics.
o If all tests normal and baby is
very well-appearing, may delay abx – discuss delay with attending.
¤ Consider specific viral tests if suggestive history. Proven
viral source makes meningitis less likely.
o Antibiotic choice: Ampicillin PLUS either Gentamicin OR
Cefotaxime (Claforan)
¤ Coverage for E.
Coli and GBS
¤ Enterococcus
(gram+ in urine) and Listeria (rare) require Ampicillin
¤ If meningitis
suspected, use Amp and Cefotaxime
o Add acyclovir if HSV risk factors present
á
If LP is unsuccessful- carefully
consider giving antibiotics v. observation without them:
o Obtain CRP or procalcitonin
o If infant ill-appearing or inflammatory marker high,
consider empiric antibiotics with repeat LP attempt after hydration
o If infant well-appearing and inflammatory marker low,
consider observation without antibiotics
PATHWAY FOR INFANTS 29-60 DAYS
Infants immunized <48 hours prior to
onset of fever should be considered individually
á
Ill-appearing infant
with no source of fever:
o proceed with complete work-up above, start empiric antibiotics.
á Well-appearing infant with no source of fever:
o Urinalysis by any method. If positive, cath gram stain and
urine culture
¤ ÒpositiveÓ = LE present OR >4 WBC
o Blood cultures x2
o Procalcitonin or CRP or WBC with Diff
o High risk criteria:
¤ WBC <5,000 or >15,000
¤ Total bands >1500
o If low risk, can observe without LP and without antibiotics
¤ If close follow-up assured and PCP in agreement, may d/c
home
o If not low risk,
admit for observation and strongly consider LP. Do not give antibiotics without doing LP
¤ Temp < 101.5 or positive viral tests = very low risk for
bacterial meningitis. Consider focused viral testing if suggestive history or
exam
á
Antibiotic choice, if
used:
o Ceftriaxone 75mg/kg (100 mg/kg meningitic dosing) is safe
in babies >28 days
o If gram+ in urine,
must use ampicillin to cover enterococcus
These
are only guidelines that must be individualized based on clinical experiences
and circumstances.
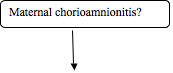
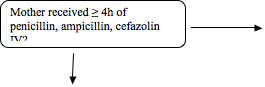
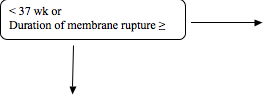
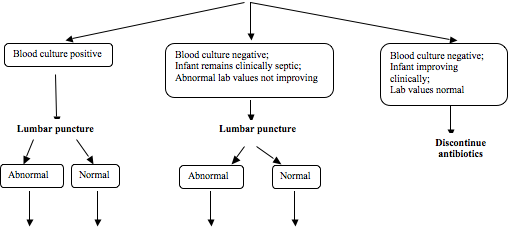
Neonatal (NICU) Sepsis Pathways
Neonatal Early Onset
Sepsis Algorithm
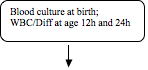
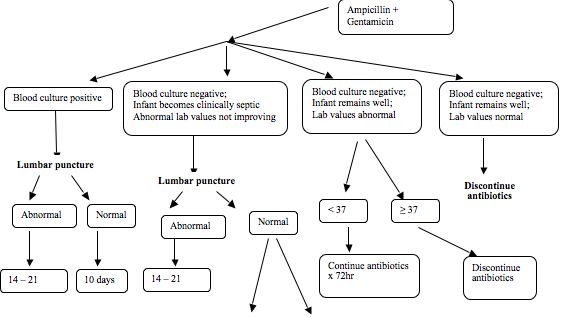
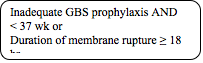
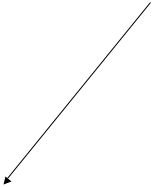
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
Pathway A
![]()
![]()

![]()
![]()
![]()
![]()
Pathway B
![]()
![]()
![]()
![]()
![]()
![]()
Pathway C
![]()
![]()
![]()
![]()
Treatment Recommendations
|
Empiric therapy |
Ampicillin + Gentamicin |
|
- if renal insufficiency |
Ampicillin + Cefotaxime |
|
Positive blood culture w/ no identifiable focus or underlying cause |
Targeted therapy x 10 days |
|
Culture negative but clinical status warrant treatment |
Ampicillin + Gentamicin x 3-7 days |
|
Meningitis attributable to gram-negative organism |
Cefotaxime x 21 days or 14 days from 1st negative culture, whichever is longer |
|
Uncomplicated meningitis attributable to Group B streptococcus (GBS) |
Penicillin G or Ampicillin x 14 days from 1st negative culture |
|
Uncomplicated culture negative meningitis |
Ampicillin + Gentamicin x 14 days |
Meningitis
CLINICAL MANIFESTATIONS
- Infants: non-specific signs
- Symptoms: Fever, irritability, lethargy, poor feeding, high pitched cry.
- Signs: Lethargy, inconsolability, bulging fontanel, seizure
- Over 12 months:
- Symptoms: fever, headache, stiff neck, AMS
- Signs: KernigÕs sign, BrudzinskiÕs sign, photophobia, somnolence
PHYSICAL EXAM
*wear a mask if you are considering bacterial meningitis!
- Complete exam with particular attention to:
- Neuro exam: pupils, reflexes, tone, mental status
- Neck stiffness, KernigÕs, BrudzinskiÕs
- Rash: purpura/petechiae, viral exanthem
LABS AND IMAGING
á If considering bacterial meningitis:
o CBCd – for all cell lines, any signs of DIC
o CRP – to trend
o Blood cultures x2
o BMP to monitor for SIADH and to have serum glucose prior to LP
o LP with routine studies, culture (compare CSF glucose to serum)
¤ If signs of ICP (including high BP) or if focal neurologic signs, head CT prior to LP
á Possible studies based on presenting history:
o Throat culture
o Stool culture
o HSV PCR on CSF, blood
BACTERIAL CAUSES OF MENINGITIS
|
Age Group |
Pathogens |
|
Newborn Empiric
Abx options: á
ampicillin + cefotaxime á
ampicillin + gentamicin |
|
|
4-12 weeks Empiric
ABx : á
Ampicillin and ceftriaxone |
|
|
Over 12 weeks Empiric
Abx: á
Ceftriaxone |
|
**add
vancomycin if VP/VA shunt, if critically ill, if gram+ organisms in infant
>12 weeks
**add
doxycycline if concern for Rickettsial disease
CEREBROSPINAL FLUID ANALYSIS
|
Indices |
Normal |
Bacterial¹ |
Viral |
Fungal |
TB |
|
Cell Count |
Pre-term: 0-25 Term 0-30 days: 0-22 Child: 0-7 |
100-20,000 |
10-3,000 |
variable |
100-500 |
|
Cell Type |
Neonate: polys. Child: lymphs |
PMN |
Lymphs2 |
Lymphs |
Polys early, then Lymphs/Monos |
|
Glucose (mg/dl) |
>40 or > ½ serum glucose |
<40 or <½ serum glucose |
Normal |
Decreased |
Decreased |
|
Protein (mg/dl) |
Preterm: 65-150 Term: 20-170 Child: 5-40 |
Elevated |
Elevated but less than 200 |
Elevated |
Markedly Elevated |
|
Gram Stain |
Negative |
Positive |
Negative |
Varies |
Negative |
¹In partially treated bacterial meningitis, CSF findings may resemble viral meningitis.
2 In viral meningitis, PMNs predominate initially, then lymphocytes appear.
Repeat LP in 48 hrs in:
á Neonatal meningitis
á Pneumococcal meningitis
á Gram (-) organism
á No improvement on initial therapy
COMPLICATIONS
á SIADH
á Septic Shock and DIC/Coagulopathy
á Cerebral Edema
á Neurologic findings, both transient and persistent:
o Cranial nerve palsies (esp. CN VI)
o Hearing loss (from infection or from aminoglycoside, if used)
á Subdural effusions and empyema
á Hydrocephalus: communicating or obstructive
á Bacteremia with resultant septic arthritis, pericarditis, and pneumonia
á Seizures: usually in first 48 hrs
o Consider EEG, CT for any seizures after 48-72 hours or focal seizures – may indicate intracranial sequelae (abscess, infarct, cerebral edema).
Urinary Tract Infections
DEFINTION
- Defined as significant bacteruria WITH pyuria – evidence of inflammatory response
- Pyuria: positive nitrites on a dip or >5 WBC on micro
- Significant bacteruria defined:
- >50,000 CFU of pathogenic bacteria on catheterized urine
- >100,000 CFU of pathogenic bacteria on clean-catch urine
- Not reliable – never
culture a bag urine
- >1000 CFU of pathogenic bacteria on suprapubic aspirate
á Asymptomatic bacteruria: bacteria present without pyuria
o NOT a UTI, does NOT require treatment in otherwise healthy child
RISK FACTORS FOR UTI
- Uncircumcised Male
- Bacterial colonization – i.e. from indwelling catheter/suprapubic catheter
- Urinary stasis, obstruction, or reflux
- Urethral or vaginal foreign body
- Dysfunctional voiding/constipation
- Previous UTI
- Sexual practice/abuse
PRESENTATION
¤ Younger children (<2yrs):
o Fever >2 days with no other source
o Suprapubic tenderness
o Concern if: prior UTI, urogenital abnormality, uncircumcised boy
¤ Older children:
o Dysuria, frequency, urgency
o Abdominal pain, suprapubic tenderness, flank/back pain/tenderness
o Fever (less common)
¤ Concern for pyelonephritis:
o Fever, vomiting, flank tenderness
ORGANISMS ASSOCIATED WITH UTI
Gram negative
- E. coli, Klebsiella, proteus, enterobacter, pseudomonas
Gram positive
- Enterococcus and Group B strep
(neonates), staph saprophyticus (teen girls), coag-negative staph,
staph aureus
MANAGEMENT
¤ Full H&P with attention to predisposing factors for UTI:
o Assess risk factors above
o GU anomalies, labial adhesions, abdominal masses, sacral dimple/tuft, LE reflexes and tone
o Blood pressure, growth curve
¤ Obtain UA, gram stain, culture if UTI suspected
o Negative dip, well-appearing patient: send culture, do not treat with abx
o Positive dip, well-appearing patient: treat empirically, follow culture/sensitivity
¤ Indications for admission of ill-appearing patient:
o Dehydrated, not tolerating PO intake
o Known kidney disease or urologic abnormality
o Immunocompromised
o All infants <60 days – consider blood cultures, empiric abx IV
o Young child with unreliable follow-up
o Failure to respond to outpatient treatment
¤ Inpatient management:
o Check BMP for lytes and renal function
o IV fluids if not tolerating PO intake
o Empiric antibiotics pending culture (based on gram stain)
ANTIBIOTIC CHOICE
**for patients >60 days. See Òinfant with
feverÓ section for patients <60 days**
¤ Inpatient empiric therapy: Ceftriaxone
o Special cases: recurrent UTI, age <60 days – consider individually
o Gram positive: add ampicillin until enterococcus ruled out
¤ Outpatient empiric therapy: cefdinir (Omnicef), TMP-SMX are good initial choices
o Base on local sensitivities, if known
o Always follow gram stain, culture to change abx as indicated
¤
** follow-up culture for test of cure is NOT indicated in
simple UTI
¤ Antibiotic prophylaxis: controversial. Decision made in consultation with nephrologist or urologist.
INDICATIONS FOR IMAGING
¤ Renal Ultrasound:
o First UTI age <2 years
o Slow response to IV abx (fever >48 hrs, no clinical improvement)
o Recurrent UTIs
o UTI with poor growth, abnormal kidney function, or HTN
o *consider in patient with UTI, strong family hx of VUR
¤ Voiding Cystourethrogram (VCUG)
o Any of the above conditions with abnormal renal US
o **VCUG can be done while inpatient for treatment of acute UTI
Parapneumonic Effusion and Empyema
DEFINITION AND CLASSIFICATION
á Parapneumonic effusion : pleural fluids associated with pneumonia
o uncomplicated, free-flowing effusion = without loculation
o complicated effusions = with loculation
o consider this diagnosis if no improvement after 48 hrs antibiotics for pneumonia
¤ still febrile, persistent respiratory distress, clinically unwell
COMMON CAUSES OF PLEURAL EFFUSIONS
- Pneumonia
- Trauma (also hemothorax)
- Malignancy
- Fluid overload (heart disease ˆ CHF, kidney disease ˆ fluid retention)
- Immunodeficiency disorders (complicated PNA)
- Adjacent infection involving the esophagus, mediastinum, abdomen ˆ reactive effusion
COMMON ORGANISMS
á Streptococcus pneumonia, strep pyogenes
á Staphylococcus aureus - think about this if pneumonia superinfecting influenza!
á Haemophilus influenzae
á Anaerobes
DIAGNOSTIC WORKUP AND MICROBIOLOGY
- Ultrasound: sensitive for effusion, best imaging to identify loculations
- If large, loculated effusion, consider CT chest to r/o intraparenchymal abscess
- CXR – PA +/- lateral decubitus (layering can be seen, may help dx)
- Blood cultures should be performed in all patients with parapneumonic effusion
- All
cases should be treated with intravenous antibiotics – empiric
coverage for above organisms or guided by cultures
SURGICAL PROCEDURES
- Chest tube placement – small ÒpigtailÓ for simple effusion or larger tube for complex. Can be placed by surgeon or PICU attending.
- Can infuse tPA through chest tube to break up loculations, avoid VATS
- VATS (video assisted thoracoscopic surgery) - Achieves debridement of fibrinous material, break down of loculations, and drainage of pus/fluid from the pleural cavity under direct visualization.
- Decortication- Open thoracotomy and excision of the thick pleural rind with evacuation of fluid. Longer, more complex, more invasive than VATS.
MANAGEMENT PROTOCOL FOR PARAPNEUMONIC EFFUSION
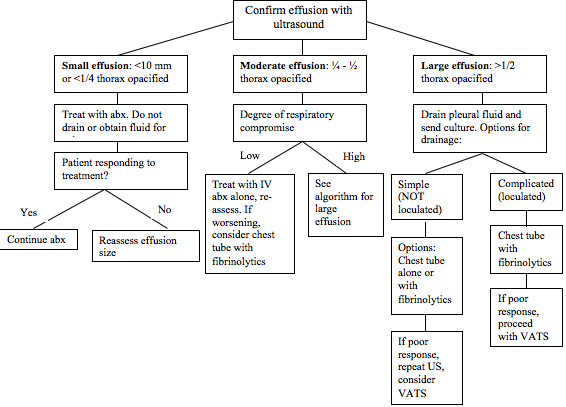
Based on the 2011 IDSA guidelines for management of parapneumonic effusion/empyema.
MRSA Infections
MRSA is increasingly a
community-acquired infection. Most common is skin/soft tissue
infection such as cellulitis, abscess.
Healthcare-acquired MRSA is also common and often has different patterns of
antibiotic susceptibility.
RISK FACTORS FOR HEALTH CARE ASSOCIATED MRSA
- Hospitalization in the past year
- Surgery in the past year
- Indwelling line or percutaneous medical device (port, broviac, PICC, suprapubic cath)
- Dialysis (hemo or peritoneal)
- Home nursing care, living in long-term care facility
ANTIBIOTIC SUSCEPTIBILITY PATTERNS
PH ChildrenÕs Hospital Antibiogram, 2014
|
% sensitive to: |
TMP-SMX |
Clindamycin |
Vancomycin |
Gentamicin |
Doxycycline |
Linezolid |
|
MRSA from
Sterile site* |
100% |
63% |
100% |
100% |
100% |
88% |
|
MRSA from
Non-sterile site** |
99% |
94% |
100% |
100% |
100% |
100% |
*sterile
site = blood, CSF, urine
**non-sterile
site = skin/soft tissue
TESTING STAPH AUREUS FOR SUSCEPTIBILITY TO CLINDAMYCIN
If lab reportsÉ. Then interpret asÉ..
Erythro susceptible, Clinda susceptible Clinda susceptible
Erythro resistant, Clinda resistant Clinda resistant
Erythro resistant, Clinda susceptible Unknown; request D test
Negative D test Clinda susceptible
Positive D test Clinda resistant
ANTIBIOTIC THERAPY FOR COMMUNITY STAPH AUREUS INFECTIONS
Outpatient- Skin and soft tissue infections without severe illness
- Empiric-
¯ Cellulitis without abscess: cephalexin or clindamycin (for staph and strep spp.)
¯ Cellulitis with abscess: Drain the abscess, send culture
á Abscess <5 cm, no cellulitis: no abx
á Abscess withcellulitis: TMP-SMX, clindamycin, or doxycycline PO
- Culture proven MRSA: base on sensitivities. First line oral abx include:
¯ Clindamycin- Ensure D-test negative if erythromycin resistant
¯ Trimethoprim-sulfamethoxazole
Inpatient
á Skin and soft tissue infections – see table
á Cellulitis with abscess, failure of outpatient abx, systemically ill (febrile, malaise) or anticipated need for drainage:
o
Culture
any drainage as soon as possible
o
If ill-appearing, consider blood
cultures
o If extensive, patient is febrile, consider imaging to rule out deep abscess or osteomyelitis, CRP to trend
¤ Suspect abscess: US or MRI, case-by-case decision
¤ Suspect osteo ˆ add vancomycin, get MRI
o If cellulitis crosses joint lines, must rule out septic arthritis
¤ MRI is imaging of choice if imaging deemed necessary
á Osteomyelitis, septic arthritis, Pneumonia:
o Vancomycin and clindamycin (clinda added for anti-toxin effect)
á Bacteremia, endocarditis: clindamycin cannot be used because it does not stay in the bloodstream.
o Abx of choice: vancomycin until sensitivities known
o Be suspicious for seeded sites: osteo, joints, endocarditis, occult abscess
DECOLONIZATION TO PREVENT RECURRENCE
Efficacy is unproven. Offer to
patients with recurrent MRSA or numerous family members with MRSA infections.
Protocol:
- Keep fingernails clean and cut short, change towels, washcloths, and sheets daily.
- Mupirocin to anterior nares BID for 2 weeks.
- Betadine skin cleanser (7.5%): wash whole body three times per week for 3 weeks
- Bleach baths- 1 tsp per gallon of water- 2 times per week.
Bite Wounds
á Most common bites: dogs (80%), cats, humans
o Dog bites: 5-10% become infected
o Cat bites: 30-50% infected
o Human bites: assume 100% infected - also consider Hep B, HIV in human bites!
Evaluation
- History:
- Provoked
v. unprovoked
- Type
of animal? AnimalÕs immunization status known? Animal quarantined?
- Patient
immunization status
- Exam:
- Location
of bite, deep puncture v superficial
- Signs
of infection (purulence, erythema, induration) or clean-appearing
- Imaging: x-ray
if foreign body is suspected or if there is apparent bone or joint injury.
Management
- Notify DHEC
– animal to be quarantined if immunization status unknown
- Initial wound
management:
- Wash
with soap, irrigate with sterile saline (may require local anesthetic)
- Examine for
vascular, joint, muscle, tendon, or nerve damage.
- Suturing
ok: Large wounds or wounds
that are on the face. Low risk of infection.
- DO NOT suture: infection risk is too high
- puncture
wounds
- wounds on the hand or feet
- wounds over 8 hours old
- Follow up
frequently
- Indications for
admission/inpatient treatment include:
- failure of outpatient oral antibiotics
- concerns for infection and delay in seeking medical
care
- systemic illness
- immunocompromised
patient
ANTIBIOTIC THERAPY
- Antibiotic
therapy is indicated in all of the following circumstances:
¯
All cat and human
bites
¯
Moderate to severe
injuries, Crush injuries, deep puncture wounds
¯
Wounds on hands, feet,
face, genitals
¯
Immunocompromised
patient (remember asplenia, DM qualify)
¯
Bites >8 hours old
at first evaluation (consider wound culture)
¯
Any signs of infection
(obtain wound culture)
á
Specify type of bite.
Eikenella and pasteurella are hard to ID.
- Antibiotic
regimen of choice for animal OR human bites: see table
TETANUS PROPHYLAXIS
|
|
Clean/Minor
Wounds |
Other
Wounds |
||
|
Previous
number tetanus toxoid doses (DTaP, TdaP) |
Td1 |
TIG |
Td1 |
TIG |
|
Unknown or <3 |
Yes |
No |
Yes |
Yes |
|
³ 3 previous doses |
No2 |
No |
No3 |
No |
1For children <7 yo, give DTaP unless otherwise
contraindicated. For persons ³ 7
yo, give Td.
2Yes, if it has been >10 years since the last dose.
3Yes, if it has been >5 years since the last dose.
RABIES PROPHYLAXIS
- Rabies Immune
Globulin (RIG) given on day 1.
- 20 IU/kg, half infiltrated into the
wound, half given IM.
- Do
not give if patient has previously had rabies vaccine.
- Rabies Vaccine
given IM on days 3, 7, 14, and 28.
- Requires
contacting DHEC.
|
When
to Give Rabies Prophylaxis |
|
|
Clinical
Scenario |
Approach |
|
Dog, Cat, or Ferret Bite Animal is healthy and
available for observation. |
Rabies prophylaxis if the
animal develops symptoms of rabies |
|
Dog, Cat, or Ferret Bite Animal is rabid or rabies is
suspected. |
Administer immunization and
RIG |
|
Dog, Cat, or Ferret Bite Unknown status of animal |
Consult DHEC |
|
Skunk, Raccoon, Bat, Fox,
Woodchuck, or other Carnivore Bite |
Consider the animal rabid
unless proven otherwise or in an area free of rabies. Administer immunization and
RIG. |
|
Livestock, Rodent, or Rabbit
Bite |
Generally not considered
rabid. Consult DHEC. |
Empiric Therapy of Skin and Soft Tissue Infections
|
Condition |
Common Pathogens |
Recommended Empiric Treatment |
Alternative Treatment |
Duration of Therapy |
|
Impetigo/ Ecthyma |
-Beta hemolytic
streptococci -S. aureus |
Cephalexin Mupirocin topical |
Clindamycin PO Sulfamethoxazole/Trimethoprim
PO Doxycycline PO** |
7 days |
|
Purulent SSTIs (Cutaneous abscesses,
furuncles, carbuncles, and inflamed epidermoid cysts) |
S. aureus |
Mild: no
systemic signs of infection, abscess < 5cm - I&D |
n/a |
n/a |
|
Moderate:
localized infection, abscess > 5cm - I&D -
Sulfamethoxazole/Trimethoprim PO |
Doxycycline PO** |
7 days |
||
|
Severe:
failure of oral antibiotics, immunocompromised, or systemic signs of
infection - I&D - Clindamycin IV |
Vancomycin IV Linezolid IV or PO Clindamycin PO |
7 days |
||
|
Non-purulent SSTIs (Erysipelas and cellulitis) |
-Beta hemolytic
streptococci -S. aureus |
Mild: no
systemic signs of infection - Cephalexin |
Clindamycin PO |
5 days |
|
Moderate: systemic
signs of infection - Cefazolin - Nafcillin |
Clindamycin IV or PO |
7 days |
||
|
Severe:
penetrating trauma, history of MRSA, purulent drainage, immunocompromised - I&D - Clindamycin IV |
Vancomycin IV Clindamycin PO |
10 days |
||
|
Necrotizing Fasciitis |
Polymicrobial |
- Surgical intervention - Vancomycin IV +
Piperacillin/Tazobactam + Clindamycin |
For piperacillin/tazobactam
alternative: - Meropenem - Ceftriaxone +
Metronidazole - Fluoroquinolone +
Metronidazole For documented group A
strep: - Penicillin + clindamycin |
varies |
|
Clostridial Myonecrosis (Gas Gangrene) |
-Clostridium species |
- I&D - Vancomycin +
Piperacillin/Tazobactam |
For piperacillin/tazobactam
alternative: - Meropenem For definitive therapy: - Penicillin + clindamycin |
varies |
|
Pyomyositis |
-S. aureus |
Immunocompotent: - Drainage - Clindamycin IV |
For clindamycin
alternative: - Vancomycin - Linezolid For piperacillin/tazobactam
alternative: - Meropenem - Ceftriaxone +
Metronidazole - Flouroquinolone +
Metronidazole For MSSA - Nafcillin |
21 days |
|
Immunocompromised: - Drainage - Clindamycin IV +
Piperacillin/Tazobactam |
||||
|
Surgical Site Infections *if
significant systemic response* |
48hr – 4 d: -S. pyogenes -Clostridium species |
- Suture removal - Incision and drainage - Penicillin + clindamycin |
n/a |
varies |
|
> 4 days: -S. aureus |
- Suture removal - Incision and drainage - Vancomycin - Clindamycin |
For MRSA - Linezolid For MSSA - Cefazolin |
||
|
GI, GU, Perineum, Axilla: -Gram negatives -Anaerobes |
- Suture removal - Incision and drainage - Ceftriaxone +
metronidazole |
For ceftriaxone
alternative: - Levofloxacin |
||
|
Bites |
Dogs or cats: -Pasturella -Anaerobes |
- Amoxicillin/clavulanate - Ampicillin/sulbactam |
- Cefuroxime +
metronidazole - Septra + metronidazole - Levofloxacin +
metronidazole - Doxycycline PO** |
5 days |
|
Humans: -Streptococci -S. aureus -Eikenella -Anaerobes |
- Amoxicillin/clavulanate - Ampicillin/sulbactam |
- Levofloxacin +
metronidazole - Doxycycline PO** |
||
|
Cat Scratch Disease |
-B. henselae |
- Azithromycin |
n/a |
5 days |
*significant systemic response is defined as erythema and induration extending greater than 5cm from the wound edge, temperature >38.5C, HR>90, WBC >12,000/microliter or <400/microliter, or tachypnea >24 breaths per minute.
**Doxycycline is not recommended in patients younger than 8 years old
Central Line-Associated Bloodstream
Infections
MAJOR PATHOGENS
- Gram positive: coagulase negative Staph (i.e. S. epidermidis)
= most common.
- Also
MSSA, MRSA, Streptococcus species, enterococcus
- Gram negative:
E. coli, Klebsiella, Acinetobacter, Enterobacter, Pseudomonas
- Fungi: Candida
species
DIAGNOSIS
- Patient with
central line and fever or cellulitis/purulence around line site:
- Obtain
central line and peripheral (percutaneous) blood cultures
- Culture
any drainage from the catheter site
MANAGEMENT
Simple Exit Site
Cellulitis in immunocompetent patient:
- If afebrile,
well-appearing, limited cellulitis:
- Culture the line,
start oral abx (clindamycin)
- Daily
follow-up to monitor
- If blood
culture positive or if any progression on oral abx,
admit for IV abx.
Fever,
significant skin/soft tissue infection, or ill-appearing:
á
Admit, obtain central
line and peripheral blood culture, start empiric abx:
o Vancomycin + cefepime
¤ Review past culture/sensitivities if previous line
infections
o Add fungal coverage if clinically septic AND one of:
¤ TPN through line, hx prolonged abx use, patient with
leukemia, s/p bone marrow or organ transplant, hx candida infection
o Anti-fungal choice:
¤ Fluconazole if no azole exposure in previous 3 months
¤ Micafungin if recent azole exposure
á
If blood culture becomes positive, repeat daily until a
culture remains negative for 48 hrs. Duration of treatment starts from first
negative culture.
When
to remove the Central Line: See table below. General guidelines:
á
Short-term line (i.e.
PICC for 2-4 weeks) should be removed if infected.
á
Long-term lines should
be removed if:
o Endocarditis, septic thrombophlebitis, or metastatic
infection
o Tunnel infection or port abscess
o Blood cultures continue to be positive >72 hrs after abx
started
o Infection with S. aureus, pseudomonas, fungus, mycobacteria
Antimicrobial
Locks: When treating through the infected
line. Common: vanc, gent, ethanol
á
Antibiotic instilled
into lumen of catheter when not in use. Continued for duration of IV abx,
sometimes longer. Guidelines on
phformulary.net. Requires ID consult
á
Some patients require
chronic prophylaxis with ethanol locks.
Pathogen-Specific Therapy for Central Line-Associated Infection
|
Intravascular Device |
Complicated / Uncomplicated |
Organism |
Catheter/Port Removed (y/n) |
Antimicrobial Therapy |
Duration |
|
Short-term CVC or AC |
Uncomplicated |
CoNS |
Y |
Nafcillin or Vancomycin |
5-7 d |
|
Staphyloccus aureus |
Y |
Nafcillin or Vancomycin |
³ 14 d |
||
|
Enterococcus |
Y |
Ampicillin or Vancomycin |
7-14 d |
||
|
Gram (-) Rods |
Y |
Systemic |
7-14 d |
||
|
Candida |
Y |
Fluconazole (Micafungin if C. glabrata or C. krusei) |
14 d |
||
|
Complicated |
- |
Y |
Systemic |
4-6 w |
|
|
Long-term CVC or Port |
Uncomplicated |
CoNS |
N |
Nafcillin or Vancomycin +
Vancomycin Lock |
10-14 d |
|
Staphyloccus aureus |
Y |
Nafcillin or Vancomycin |
³ 14 d |
||
|
Enterococcus |
N |
Ampicillin or Vancomycin +
Ampicillin or Vancomycin Lock |
7-14 d |
||
|
Gram-negative Bacilli |
Y |
Systemic |
7-14 d |
||
|
N |
Systemic + Ceftazidime or
Gentamicin Lock |
10-14 d |
|||
|
Candida |
Y |
Fluconazole (Micafungin if C. glabrata or C. krusei) |
14 d |
||
|
Tunnel Infection or port
abscess |
- |
Y |
Systemic |
7-10 d |
|
|
Septic thrombosis,
endocarditis, or osteomyelitis |
- |
Y |
Systemic |
4-6 w |
Empiric Therapy for Intra-Abdominal Infections
|
Infection |
Type |
Treatment |
Duration |
|
Complicated Intra-abdominal Infections |
Community-acquired |
1.
Ceftriaxone + Metronidazole 2.
Cefoxitin |
7
days following source control |
|
Community-acquired:
Immunocompromised |
Cefepime + Metronidazole |
||
|
Health
care-associated |
Piperacillin/Tazobactam
+ Fluconazole +/-
Vancomycin* *if high risk of MRSA |
||
|
Biliary Infections |
Community-acquired
cholecystitis: Mild
to moderate |
Ceftriaxone |
Varies;
dependent on surgical intervention |
|
Community-acquired
cholecystitis: Severe
or Immunocompromised |
Cefepime
+ Metronidazole |
||
|
Cholangitis |
Cefepime
+ Metronidazole |
||
|
Health
care-associated |
Piperacillin/Tazobactam |
||
|
Appendicitis |
Perforated |
1.
Ceftriaxone + Metronidazole 2.
Cefoxitin |
7
days following source control |
|
Non-perforated |
3
days following source control |
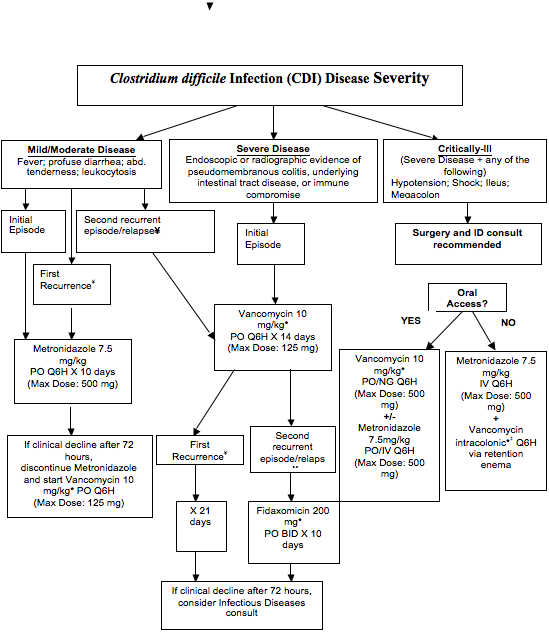
ChildrenÕs Hospital Clostridium difficile Infection Management
Notes
* Indicates CH Antimicrobial Stewardship Program (ASP) restricted medication (oral and intracolonic vancomycin; fidaxomicin). Approval required - (ASP Pager) 352-1461.
à Intracolonic vancomycin pediatric dosing: 250mg in 50mL for 1-3 years of age; 375mg in 75mL for 3-9 years of age; 500mg in 100mL for 10 years of age and older
Æ CDI high-risk antibiotics include: beta-lactams, fluoroquinolones, clindamycin
¤ The C. difficile PCR
assay is a real-time in vitro diagnostic test for the direct,
qualitative detection of C. difficile toxin B gene in specimens from
patients suspected of having C. difficile
associated disease. (with > 90% sensitivity and specificity)
´
Recurrence/relapse is limited to 90 days from initial episode. Onset beyond this threshold should be
treated as initial episode
C. diff Laboratory
Diagnostics:
á Clostridium difficile Toxin B by PCR¤
á If C. difficile PCR (-), discontinue therapy and re-evaluate source of
infection.
á Repeat testing is not
indicated for proof of cure and is not recommended.
á Nursing:
o
Sample
should be unformed or watery stool; formed stool should not be sent for PCR
testing
o
Refer
to Infection Control policy for contact isolation and hand washing for suspected
or proven CDI
Additional Orders:
á Discontinue bowel
regimens including stool softeners, laxatives, antiperistaltic agents (e.g.
docusate, sennosides, loperamide, metoclopramide, polyethylene glycol)
á Physician must address
acid-suppressing agents such as proton-pump inhibitors (PPIs) (e.g.
esomeprazole) or H2-receptor antagonists (H2s) (e.g. ranitidine, famotidine)
o
Discontinue
ALL acid-suppressing agents
o
Discontinue
PPI and initiate alternative therapy (e.g. ranitidine, sucralfate)
o
Continue
PPI. Physician to document
indication (e.g. active GI bleed)
á Discontinue concomitant antimicrobial therapy to reduce the risk of CDI. If the patient must remain on antibiotics, de-escalate/change to an antibiotic that is low-risk for CDI such as: aminoglycosides, tetracyclines, macrolides, sulfonamides (SMX-TMP).
á Please contact ASP at (Pager) 352-1461 for assistance.
Shunt Infections
á
Most infections within
1 month of shunt placement but can occur any time
á
Skin flora (s.
epidermidis) most common; also s. aureus, enteric organisms
CLINICAL MANIFESTATIONS
- Signs/sx of CNS
infection:
- Fever,
irritability, somnolence, AMS, seizure, tenderness over shunt tubing,
headache
- Signs/sx of
increased ICP due to malfunction:
- Elevated
BP, fixed downward gaze, pupillary abnormalities, somnolence, lateral
rectus palsy, prominent scalp veins
- LATE
finding: CushingÕs triad
- Peritoneal signs
can develop
DIAGNOSIS
á
Diagnosis requires CSF
culture
á
Consult neurosurgery
– neurosurgeon will decide on LP vs. tapping the shunt
o Shunt tap localizes infection to the hardware and is
usually the test of choice
á
Send CSF for routine
indices, culture
TREATMENT
Regimens include:
á
Vancomycin +
Ceftazidime
á
Vancomycin +
Gentamicin
á
Vancomycin +
Ceftriaxone (no pseudomonas coverage)
*Vanc trough goal
15-20
**never use clindamycin for staph coverage in CNS – it
does not penetrate the CSF!
Decision to treat through the infection or remove the shunt
based on organism, clinical status, neurosurgery
recommendation.
á
Shunt may be
externalized to external ventricular drain until infection cleared
Respiratory and Allergy
Asthma
DEFINITION
A chronic disease of recurrent, reversible airway obstruction. It is characterized by smooth muscle spasm, mucosal inflammation, and mucus hypersecretion.
DIFFERENTIAL DIAGNOSIS OF WHEEZING
Not all that wheezes
is asthma!
á Infectious: bronchiolitis, pneumonia
á Anatomic: vascular ring/sling, mediastinal mass, aspirated/ingested FB, congenital airway abnormality
á Pulmonary: bronchiectasis (CF, PCD), interstitial lung disease, ABPA, WegenerÕs
á Cardiac: CHF/pulmonary edema from CHD or cardiomyopathy, anatomic abnormalities
á GI: GERD
HISTORY – specific to asthma dx
- When diagnosed, past hospitalizations (floor and PICU), past intubations/need for BiPAP
- How many oral steroid bursts in last year? ED visits?
- Current medications? Has pt run out? Compliance?
- Baseline symptoms:
- Average number of times using albuterol per week (>2/wk = poor control)
- Night-time awakenings (>2/month = poor control)
- Asthma triggers: weather changes, allergens, colds, exercise, smoke, worst season
- Comorbid conditions: GERD, chronic sinusitis, allergic rhinitis, ABPA, OSA (snoring?)
PRESENTING
SYMPTOMS
Not all asthma
presents as wheezing! Other presentations:
- Dyspnea with little provocation
- Chronic cough
- Exercise intolerance
- Chest tightness/pain
- Night awakenings
- Recurrent croup, pneumonia, or ÒbronchitisÓ
PHYSICAL EXAM
- General appearance/work of breathing:
- accessory muscle use, retractions, nasal flaring, grunting, unable to speak full sentences, anxiety/agitation/ lethargy, cyanosis/signs of poor perfusion
- Vital signs:
- Tachycardia (from distress or Beta agonist use), Pulsus paradoxus (reduction of systolic BP more than >10mmHg during inspiration – late and serious finding)
- HEENT:
- nasal polyps, allergic shiners, Morgan Dennie lines, conjunctival cobblestoning
- Respiratory:
- Inspiratory/expiratory wheezing. Rales/rhonchi, prolonged expiratory phase
- Wheezing may not be heard with poor air exchange.
- Skin: cyanosis
LABORATORY EVALUATION
- Acute exacerbation:
- Unless toxic or febrile, mild-moderate exacerbation does not require labs/imaging
- CBG/ABG: if significant distress, to evaluate ventilation (PaCO2). Interpret PaCO2 in light of resp rate. Significant WOB + normal PaCO2 = concerning
- CXR: consider if febrile, if focal exam, if concern for PTX
- In most exacerbations, hyperinflation present. Patchy atelectasis common.
- Look for PTX, pneumomediastinum
- Potassium: Beta-agonists drive K into the cells, ˆ low serum K. Check BMP if pt will be on fluids (NPO due to WOB or on continuous albuterol)
- Chronic management:
- Pulmonary Function Testing (PFTs): obtain yearly in stable, chronic asthma or more often depending on symptoms.
TREATMENT OF
ACUTE EXACERBATION
- Oxygen
as needed
- Steroid
burst: loading dose of 2 mg/kg prednisone (tablet) or prednisolone
(liquid), then 1 mg/kg BID for total of 3-5 days
- If
NPO, use IV steroid (solu-medrol), same dose
- Albuterol:
- MDI
with spacer equivalent to neb unless pt unable to take deep breath
- Inpatient:
start 6 puffs Q2 hrs, wean per protocol (below)
- Severe
exacerbation or poor response to 6 puffs: hour-long albuterol neb 0.5
mg/kg to max 20 mg
- Can
do one hour-long neb on the floor. If need for more, transfer to PIICU
or PICU
- Ipratropium
(Atrovent): Anti-cholinergic, dilates larger airways
- For
use in ED or PICU. Do not continue after admission to gen peds.
- SEVERE
acute exacerbation: consider the following if continuous albuterol needed
- indicates PICU admission:
- Magnesium
– smooth muscle relaxer. 50 mg/kg to max 2g. Requires cardiac
monitor.
- Terbutaline
– subcutaneous beta-agonist. Uncommonly used.
INPATIENT GENERAL PEDIATRICS ASTHMA PROTOCOL
á This protocol is started once the resident deems it the appropriate level of care (general peds floor). Does not apply to PICU.
á All patients should be started on steroid burst (see above)
o Continue home controller medication to emphasize importance of daily use
á RT assesses the patient on admission and assigns a score (WARM score below).
á 6 puffs MDI with spacer given Q2 hours x2 before spacing out.
á RT (resident as well, if available) assesses patient 2 hours after 2nd treatment and assigns WARM score.
o If score 0 or 1, treatments are spaced out by one hour
o If score >1, treatments continue Q2 hours
o If score 4+, RT will notify resident immediately
á Patient considered ready for d/c when stable on Q4hr albuterol, with close follow-up.
á All patients need an asthma action plan at discharge.
WARM Score:
|
Category |
Severity |
Score |
|
Wheeze |
None |
0 |
|
End expiratory |
1 |
|
|
Entire expiratory/any inspiratory |
2 |
|
|
|
||
|
Air Exchange |
Normal |
0 |
|
One area decreased |
1 |
|
|
Multiple areas decreased |
2 |
|
|
|
||
|
Respiratory Rate |
Normal |
0 |
|
Tachypneic for age |
1 |
|
|
|
||
|
Muscle Use |
None |
0 |
|
Subcostal/intercostal/suprasternal |
1 |
|
|
Any neck or abdominal |
2 |
|
Bronchiolitis
DEFINITION/ETIOLOGY
á A clinical syndrome in children <2 yrs characterized by URI symptoms progressing to lower respiratory symptoms, including wheezing, rales/crackles, and respiratory distress of varying severity.
o Viral infection of bronchioles ˆ inflammation, edema, sloughing of dead cells, increased mucus production ˆ bronchiolar obstruction ˆ increased WOB, wheezing, crackles on exam
á Viral pathogens: RSV, rhinovirus, parainfluenza, influenza, human metapneumovirus, adenovirus, bocavirus
á Risk factors:
o Prematurity, chronic lung disease, congenital heart disease
o Young age (esp. <12 weeks)
o Immune deficiency
o Anatomic pulmonary defect
á Differential diagnosis:
o Young infant with wheezing: vascular rings/slings, CHF from congenital heart disease
o Older infant/toddler with wheezing: foreign body aspiration, aspiration pneumonia, recurrent viral-triggered wheezing, CHF, rings/slings, asthma
EVALUATION
Bronchiolitis is a clinical diagnosis.
á History:
o Onset of symptoms (peak illness at days 3-5), work of breathing, activity level
¤ Any observed apnea or increasing lethargy
o Associated symptoms: fever, fever curve over time (new fever days into illness suggests possible secondary infection)
o PO intake, UOP (number of diapers)
o Interventions tried at home (saline/suction, humidifier, OTC meds, antipyretics)
o History of any risk factors above
o History of atopy: eczema, AR, family hx of this? (esp in children 1-2 yr)
o Full PMH, FH, SH – sick contacts?
á Exam: complete exam with close attention to:
o ABCs first – work of breathing, RR, O2 sat, level of alertness
o Lung exam – diffuse v focal, crackles or wheezes, change of exam after cough or suction, accessory muscle use, grunting, head bobbing
o Any sign of secondary infection (esp if fever): otitis, pharyngitis, bulging fontanel, etc
á Labs and imaging: not often needed. Bronchiolitis is a clinical diagnosis.
o CBG: If very ill appearing, concern for impending respiratory failure (lethargy, head bobbing, grunting, increasing O2 requirement and WOB)
o CXR: if focal lung findings that do not change after suction or cough, atypical fever curve
o BMP: if significant dehydration or will be NPO for WOB and will need fluids
o CRP: can be helpful if concern for secondary bacterial infection
o UA: if persistent, new, or increasing fever after 2-3 days of symptoms. UTI is most common concomitant bacterial infection
o NOT generally indicated: CBC, RSV swab, viral respiratory panel
TREATMENT
The only treatment for bronchiolitis is supportive care. Indications for admission: hypoxia, dehydration, significant WOB poorly responsive to suction, concerning history, unreliable follow-up, parent unable to fully care for child at home.
á Supplemental O2 for hypoxia
o NC/simple mask on the floor
o High-flow NC (vapotherm), CPAP/BiPAP, ventilator in PICU
á Nasal saline and suction for congestion and work of breathing
o Use bulb as much as possible
o Wall suction with Òneo-suckerÓ and nasotracheal suction if significant distress
á Fluids if poor PO intake leading to dehydration
Inpatient management
with bronchiolitis guideline
á RT assesses patient on admission and assigns score (see ÒWARMÓ score table in asthma section)
o Score </= 2: no intervention
o Score >/=3: nasal saline and bulb suction, wait 5 minutes, score again
¤ If score still >/=3, give 3% saline neb Q4 x3. Do this even if little apparent response to first neb. Then , if score has decreased by 2, space to Q6 x2, then stop.
¤ If score increases (worsens) by 2 after 3% saline, add albuterol 2.5 mg to all subsequent treatments. (saline can induce bronchospasm), continue as above.
á
**the following patients
should ALWAYS receive albuterol with a 3% saline neb:
o Patients with CLD/BPD
o History of wheezing prior to this episode of
bronchiolitis (usually >1 yr old)
á
Resident can order interventions outside the
guideline based on the individual patient.
Cystic Fibrosis
DIAGNOSIS OF CF
Newborn screening with immunoreactive trypsinogen: Changing in 2016. New process:
á Top 4% of IRT levels will be sent for genetic testing. This is a floating cut-off but it eliminates the extra time needed to repeat the screen prior to genetic testing.
Diagnosis requires:
á One of the following:
o Presence of one or more characteristic clinical features
o Family history of CF
o Positive neonatal screening test
AND evidence of CFTR abnormality – one of:
- Sweat chloride ³60mmol/L (mEq/L) on 2 occasions
- <6 months old: 30-60 mmol/L is indeterminate. Consider obtaining genotype.
- Mutation analysis with 2 characteristic alleles
- Increased nasal transmembrane potential differences
CLINICAL PRESENTATION
Consider CF in patients presenting with these findings:
C Cough worsening/chronic cough
F Fever/FTT
P Pulmonary Function Tests decreased/Pancreatic Insufficiency
A Appetite decreased/Alkalosis
N Nutritional failure/Neonatal meconium ileus or nasal polyps
C CBC abnormality/Clubbing
R Radiographic changes/Rectal prolapse
E Exam (increased rales, wheezes, tachypnea, retractions)/Electrolyte abnormalities
A Activity decrease/Absent vas deferens
S Sputum changes/Sputum with Staph or Pseudomonas
COMPLICATIONS
Pulmonary: the
major cause of morbidity and mortality. Acute exacerbations worsen chronic
disease.
- Bacterial infection: S. aureus, H. flu, Pseudomonas, B cepacia, Acenitobacter, Stenotrophomonas, Non-tuberculous mycobacteria, many others
- Lungs colonized ˆ chronic infection, bronchiectasis, obstructive lung disease
- Asthma: a comorbidity in 25-50%
- Pneumothorax: 5-10%
- Allergic Bronchopulmonary Aspergillosis: 5-10%.Wheezing, rusty sputum, pulmonary infiltrates, eosinophilia, elevated IgE (usually >1000)
- Nasal polyps, pansinusitis, hemoptysis, clubbing (correlates with severity of lung disease)
- Cor
pulmonale at end stage due to chronic hypoxemia
Pancreas
- Pancreatic insufficiency – 85% of patients.
- malabsorption ˆ steatorrhea, FTT
- fat-soluble vitamin deficiency (A, D, E, K)
- A: Xerophthalmia, night blindness, dry skin
- D: osteopenia, rickets
- E: hemolytic anemia, neuropathies
- K: coagulopathy
- anemia, hypoproteinemia
- Pancreatitis is rare. It is more common in pancreatic sufficient patients.
- CF-related diabetes, glucose intolerance
Gastrointestinal
- Rectal prolapse – mostly in infants, toddlers
- GERD
- Intestinal obstruction
¯ Meconium Ileus: pathognomonic for CF. In neonates. Evaluate for this if no meconium in 48 hrs.
¯ Meconium Plug Syndrome: In neonates. Affects the large intestine. Associated with Hirschsprung Disease. Less common, less severe than meconium ileus.
¯ Distal Intestinal Obstruction Syndrome (DIOS) in older children. Partial or complete obstruction of the terminal ileum.
- Fibrosing colonopathy: postulated, but not proven complication of excessive pancreatic enzyme replacement
¯ Max safe dose: 10,000u lipase/kg/day
- Steatorrhea: suggests inadequate enzyme replacement. Dosing guidelines:
¯ Infants: 2,000-4,000 units lipase/120cc of formula or breastmilk
¯ Children <4years: 1,000 units of lipase/kg/meal, 500 units lipase/kg/snack
¯ Children >4years: 500 units of lipase/kg/meal, 250 units lipase/kg/snack
Hepatobiliary
- Fatty liver is common
- Cholestasis: clinically significant in 5% of patients
- Progression to focal biliary cirrhosis, portal HTN, and liver failure possible, uncommon
Other Clinical
Findings
- Impaired fertility in both genders
- Absent vas deferens in boys
- Electrolyte abnormalities: Low Na, K, Cl, metabolic alkalosis
- Hypertrophic
pulmonary osteoarthropathy: clubbing.
INPATIENT MANAGEMENT OF PULMONARY EXACERBATION
Pulmonary: goal is slowing progression of lung disease
- Airway clearance
- Chest physiotherapy (CPT). Vest and manual most common.
- Minimum of BID outpatient, 4x/day inpatient
- Thinning of secretions
- pulmozyme (dornase alfa) – 2.5mg neb daily/BID
- Hypertonic saline (7%) – neb BID mixed with or after albuterol (to prevent bronchospasm).
- Bronchodilators: as needed and with hypertonic saline
- 7% or 3% saline based on patient tolerance
- PFTs: on admission and every 5-7days during the exacerbation to monitor progress
- Response to therapy is indicated by improvement of FEV1 and FVC.
- Overnight pulse ox while inpatient to evaluate for hypoxemia.
- If
hemoptysis develops, check PT/PTT.
Give vitamin K if PT elevated.
Stop pulmozyme and CPT. Emergent Pulmonology
involvement if severe.
Infectious Disease
- Obtain sputum culture on admission.
- Start IV abx based on culture/sensitivity from last sputum culture (done q3 months at pulm office)
- ASP is automatically consulted
- Always double-cover pseudomonas to prevent developing resistance
- Obtain PICC line or other long-term access unless patient has a port
- Duration of abx based on PFTs and clinical course. 14-21 days common
- Many patients finish abx at home with PICC line.
GI/ Nutrition
- High-protein, double portion diet. Watch I/O.
- Regular diet for pancreatic-sufficient patients.
- Continue any home supplements or tube feeds, home enzyme replacement
- Weigh every 1-2 days while inpatient
- Monitor stools – constipation is a risk for DIOS, diarrhea/steatorrhea may indicate inadequate enzyme replacement
Acute Airway Obstruction/Stridor
DIFFERENTIAL DIAGNOSIS
á
Acute
o
Viral or spasmodic croup
¤
Viral: parainfluenza, RSV, adeno, rhinovirus. 6
mo-3 yrs. URI sx precede
¤
Spasmodic: no prodrome, rapid onset and resolution,
recurrent
¤
Hoarse voice, barking cough, insp stridor
¤
Rx: cold air or steamy air for comfort, 0.6
mg/kg decadron x1, racemic epi PRN acute distress.
o
Foreign body aspiration
¤
Most common in <3 yr old. Sudden onset or
indolent
¤
May have biphasic stridor, harsh monophonic
wheezes. May be drooling.
¤
Eval w/ neck films, upright and lateral
decubitus CXR
¤
Rx: removal with rigid bronch (surgery, NOT
pulm)
o
Retropharyngeal abscess/cellulitis –
children <4 yr
¤
Sx: URI ˆdysphagia, drooling,
tripod position, canÕt swallow, stiff neck
¤
Exam: febrile, red, swollen throat, hoarse cry,
stridor
¤
Eval: neck films. If pre-vertebral thickening on
films and sick pt, CT neck soft tissue to determine abscess v. cellulitis
¤
Rx: Clinda +/- ceftriaxone. Consult ENT for I&D if abscess. Treat medically if cellulitis
á
Pathogens: often polymicrobial. GABHS, s.
aureus, anaerobes
o
Peritonsillar abscess: adolescents.
¤
Sx: severe sore throat, fever, trismus
¤
Exam: asymmetrically enlarged tonsils, deviated
uvula, +/- cervical LAD
¤
Eval: May need CT neck soft tissue if cannot
visualize tonsils
¤
Rx: Clinda or Amox/clav (Amp/sulbactam) +/- decadron , ENT to I&D
á
Pathogens: GABHS, s. aureus, oral anaerobes
o
Epiglottitis
¤
6 mo to 10 yrs most
common age. Rare now due to Hib vaccine.
¤
Common bacterial causes: group A strep, s.
pneumo, s. aureus
¤
Sx: abrupt onset, toxic child, drooling,
dysphagia, tripod position
¤
Eval: lateral neck with Òthumb signÓ epiglottis
¤
Rx: consult anesthesia ˆ intubate in controlled
environment
á
Abx: ceftriaxone +clindamycin
o
Tracheitis
¤
Infectious complication of viral croup (also
post-tonsillectomy). URI prodrome 1-3 days ˆ sudden fever and
deterioration, dyspnea, stridor
¤
Common bacteria: s. aureus, s. pneumo, GABHS,
α-hemolytic strep, moraxella
¤
Eval: PA/lateral neck films ˆ
ragged tracheal borders
¤
Rx: maintain airway (may need intubation),
culture if possible (if ETT)
á
Empiric abx: clindamycin + ceftriaxone
o
Anaphylaxis
¤
See anaphylaxis section
o
Angioedema: congenital v. acquired
¤
Congenital: C1-inh deficiency. Rx = FFP or C1
inh (hard to find)
¤
Acquired: Infection (URI, UTI, strep), Drugs
(ACE-I, NSAIDs, aspirin, calcium channel blockers, opioids, radiocontrast),
idiopathic +/- urticaria
á
Rx: depends on etiology. Antihistamines,
steroids can help.
á
Hypocalcemia: Most often in neonates.
o
DDx: DiGeorge syndrome, maternal Vit D
deficiency, prematurity, IDM, birth asphyxia, hypomagnesemia, IUGR
o
Eval: check Ca, replete if low (20 mg/kg CaCl2
or 100 mg/kg Ca-gluconate
slowly)
á
Chronic
– more likely to need bronchoscopy/laryngoscopy to diagnose.
o
Laryngomalacia: insp stridor, improves when
prone, worse when crying. (0-6 mo)
o
Tracheomalacia: insp or exp stridor
o
GERD – acid irritates ˆ
causes laryngeal swelling.
¤
Rx: acid suppression +/- acute course of steroid
o
Subglottic stenosis - if hx intubation.
o
Vocal cord paralysis or dysfunction
¤
In neonates. Hx choking/gagging w/ feeds. May
have hx intubation, birth trauma, laryngeal nerve injury
o
Vocal cord/laryngeal hemangioma, papilloma,
tumor
¤
Eval: hemangioma on exam? Mom w/ HPV?
o
Laryngeal web or cyst
o
External compression:
¤
Vascular ring/sling - often have exp. Stridor/wheeze
b/c intrathoracic. Eval
w/ barium swallow – shows compression on esophagus that
raises suspicion
¤
Mediastinal mass
o
Anatomic: macroglossia, micrognathia, choanal
stenosis/atresia
¤
Choanal atresia: neonate who cannot breathe
while feeding, cannot pass NG
CLINICAL ASSESSMENT
History
á Onset/duration/recurrence, expiratory v inspiratory noise, change w/ position, relation to feeds
á Hx choking, drooling, URI sx, fever?
á Birth hx: premature/IUGR/IDM? Intubated? Resp distress needing support? Cardiac hx or procedures? Mom w/ HPV, vit D deficiency?
Physical Exam
á
ABCs -
Need to secure airway?
á Pattern of stridor, quality of cry (hoarse?)
o Inspiratory stridor ˆ extrathoraic origin
o Expiratory stridor ˆ intrathoracic origin (can also have wheeze)
o Biphasic stridor ˆfixed lesion
á Tonsillar size, position, asymmetry
á Position of comfort: neck hyperextension, tripoding
á Hemangiomas visible on skin
á Cardiac murmur
á Macroglossia, micrognathia, midline defects
DIAGNOSTIC PROCEDURES
** governed by clinical suspicion
Acute stridor:
á CBG if significant distress and concern for need of ventilatory support
á AP/lateral neck films
á Possibly CT neck soft tissue if concern for abscess
á CXR +/- lateral decubitus films
o Shows lung volumes. Do this if concern for FB
á Ca, Mg, albumin (or iCal) if neonate
Chronic stridor:
á Consider AP/lateral neck films and/or CXR
á Esophagram (barium swallow) – can show external compression (ring/sling or mass)
o Echo to show vascular anatomy if evidence of compression
á Bronch/laryngoscopy to visualize anatomy. Who needs a scope?
o SPECSR (history) and HIVE (physical)
¤ Severity: ParentÕs subjective impression of severity
¤ Progression of the obstruction over time
¤ Eating or feeding difficulties, aspiration, and failure to thrive
¤ Cyanotic episodes, ALTEs
¤ Sleep: obstruction causing retractions even during sleep
¤ Radiology: specific abnormalities detected by radiographs
á H: Hemangioma
á I: Intubation
á V: Voice
á E: Expiratory or Biphasic
Anaphylaxis
DEFINITION
Anaphylaxis is an immediate IGE-mediated hypersensitivity reaction. Diagnosis requires:
á Acute onset (within seconds to minutes) of an illness including two or more of the following in a patient with known allergies:
o Low BP or associated signs (syncope)
o Skin/mucosal involvement: flushing, urticaria, swollen lips/tongue)
o Respiratory compromise (wheeze, dyspnea, chest tightness)
o Persistent GI symptoms: cramping, vomiting, diarrhea
á OR, Acute onset of an illness including skin findings as above and EITHER low BP or respiratory compromise in a patient without allergy history
á Common causes: insect venoms, foods (peanuts, eggs, milk, seafood), drugs, contrast, latex.
CLINICAL FEATURES
- Sense of impending doom may proceed or accompany symptoms
- Cutaneous symptoms: feeling of warmth, itching, flushing, urticaria, and angioedema.
- Respiratory: stridor, bronchospasm, hoarseness, or dysphagia
- Gastrointestinal: nausea, vomiting, and diarrhea
- Cardiovascular: tachycardia, hypotension, shock, and death
MANAGEMENT
- ABCs.
- A: airway edema may require intubation
- B: use albuterol if wheezing despite epi.
- C: Trendelenburg position and NS bolus(es) if hypotensive despite epi
- Definitive treatment: epinephrine (1:1000) 0.01ml/kg/dose (max single dose 0.5ml) IM every 10-15minutes. Can be repeated up to 3 doses.
- If trigger was insect sting, give epi at the same site.
- If refractory, vasoactive drip (epi or dopamine)
- Adjunctive treatment:
- H1-blocker (Benadryl) 1-2mg/kg/dose po/IV/IM up to 75mg/dose q4-6hours. Continue 48-72 hrs (PO)
- H2-blocker (Zantac) 1.5mg/kg/dose (max 50mg) IV or PO q8hours
- Methylprednisolone (Solumedrol) 2mg/kg loading dose.
- May help prevent late phase reaction. One dose is sufficient.
- Observe at least 6 hours for late phase response, or until symptoms resolved.
- At discharge:
- All patients need epi autoinjector (EpiPen Jr for 15-30 kg, EpiPen for >30 kg)
- Allergy referral to determine trigger
Nephrology
Hypertension
DEFINITION
For children 1-17 years, averaging measurements on 3 separate occasions on RIGHT ARM. Always confirm a high reading with a manual BP.
- Normal BP: <90th percentile for age, sex, and height or <120/80, whichever is lower
- Pre-HTN: ³90th percentile (or 120/80, if this is lower), <95th percentile
- HTN(stage I): ³95th percentile ² 99th + 5 mmHg
- HTN(stage II): >99th percentile + 5 mmHg
For adolescents age 18-21: adult standards
á Normal BP: <120/80
á Pre-HTN: 120/80-139/89
á Stage I HTN: 140/90-159/99
á Stage II HTN: > 160/100
EVALUATION OF HYPERTENSION - CHRONIC
á Screening for elevated BP:
o Annually for all children starting at age 3
o At health maintenance visits under age 3 if:
¤ History of prematurity or congenital heart disease
¤ Known kidney disease or GU anomaly, history of recurrent UTI
o Confirm diagnosis of HTN with 3 readings on separate occasions
á Differentiate essential from secondary
o Essential:
¤ assoc w/ obesity, dyslipidemia, FHx of HTN
¤ Usually older children and teens
o Secondary – consider in:
¤ Pre-pubertal child with HTN, lack of co-morbidities or FH
¤ Stage II HTN
¤ Nocturnal HTN on ambulatory BP monitor
¤ Signs or symptoms of underlying cause
o Causes of secondary HTN: not an exhaustive list!
¤ Renal parenchymal disease (#1!) – scarring, PKD, dysplasia, GN, etc
¤ Renovascular disease (fibromuscular dysplasia, bilateral renal artery stenosis)
¤ Aortic coarctation, PDA
¤ CushingÕs syndrome
¤ Thyroid dysfunction
¤ Increased ICP
¤ Mineralocorticoid excess
¤ Collagen vascular disease
¤ Medications: sympathomimetics, stimulants, steroids, caffeine, nicotine, OCPs, anabolic steroids
á Evaluation for all patients: BMP, UA, urine microalbumin:creatinine ratio, +/- renal ultrasound
o +/- echo based on history, exam, height of BP
á Targeted evaluation based on history and physical, if concern for secondary HTN:
o Monogenic HTN: plasma renin activity, aldosterone level
o Coarctation: echo
o Lupus: ANA
o Renal artery stenosis: Doppler ultrasound/other renovascular imaging
o Pheochromocytoma: urine catecholamines
o Neuroblastoma: urine VMA, HVA
OUTPATIENT MANAGEMENT
Goal: BP <95%ile for patients with no comorbidities, <90%ile for
those with comorbidities
á Pre-HTN:
o Lifestyle changes recommended: salt restriction, exercise, weight loss
á Asymptomatic Stage I HTN
o No comorbidities: lifestyle changes alone for 6 months. If ineffective, start medication
o Comorbidities present: start medication
á Stage II or symptomatic Stage I HTN
o Start antihypertensive medication
EVALUATION OF HYPERTENSION - ACUTE
á Identify patients who require hospital admission (hypertensive urgency/emergency)
o Hypertensive emergency: acute, severe rise in BP with symptoms
¤ AMS, headache, lethargy, seizure, visual changes
¤ CHF, pulmonary edema (more common in infants)
¤ BP often well above stage II cutoff
¤ Requires PICU admission and often IV meds (nicardipine drip)
o Hypertensive urgency: acute, significant rise in BP without symptoms
¤ Requires close monitoring. IV vs. PO meds based on acuity of BP rise and underlying cause
INITIAL MEDICATION CHOICES
á Essential HTN: ACE-I, CCB most common initial choices. Example med in each class:
o ACE-I: Enalapril
¤ Initial: 0.08 mg/kg/dose, max 5 mg daily or BID. Titrate Q2 weeks to goal
¤ Max: 0.6 mg/kg/day, max 40 mg/day or 20 mg BID
¤ Available in 1 mg/mL suspension
¤ Good choice in DM or in patient with proteinuria. Slows progression.
¤ Cautions:
á
Teratogenic!
Ensure good birth control for teen girls, or use alternative medication!
á
Monitor
BMP (for Cr, K) 2 weeks after initiation or dose change, then q6 months
o CCB: Amlodipine
¤ Initial: 0.1 mg/kg/dose, max 5 mg, daily. Can increase to max 10 mg/day
¤ Available in 1 mg/mL suspension
¤ Good choice in essential HTN
¤ Side effects: edema, flushing, headache, gingival hypertrophy
á Secondary HTN:
o Often the drugs above are used.
o Specific drugs well-suited for specific indications:
¤ Monogenic HTN: aldosterone inhibitors (spironolactone) depending on exact type
¤ Renal disease: ACE-I
¤ Volume overload from acute GN: Lasix
o While evaluating cause of secondary HTN, CCB is a good choice
á Inpatient:
o Hypertensive urgency: often managed with isradipine (PO) or hydralazine (IV)
¤ Isradipine (CCB) 0.1 mg/kg/dose, max 5 mg, Q6hr PRN
¤ Hydralazine (vasodilator) 0.1-0.5 mg/kg/dose q6h to effect. Max 20 mg
o Hypertensive emergency: continuous monitoring, nicardipine drip
¤ 0.5-1 mcg/kg/min, titrate q15-30 min. Max 5 mcg/kg/min
Renal Tubular Acidosis
DEFINITION
RTA is a clinical syndrome characterized by impaired renal
acidification due to either impaired reabsorption of bicarbonate or impaired
excretion of hydrogen ions resulting in a hyperchloremic metabolic acidosis
with a normal anion gap.
- Anion Gap: AG =
Na – (Cl+CO2)
¯ normal range 10-14 mEq/L
- DDx of normal AG
metabolic acidosis
¯ RTA
¯ GI loss of bicarbonate from diarrhea, fistula, or s/p GI
surgery
- If there is a
normal AG metabolic acidosis and there are no GI losses, the diagnosis is
RTA.
CLINICAL MANIFESTATIONS
/ PRESENTATION
Depends on underlying cause which varies widely. Common manifestations include:
- FTT
- Polyuria
- Constipation/Vomiting
- Nephrocalcinosis/nephrolithiasis
- Rickets
LABORATORY EVALUATION
For all patients with RTA (non-AG metabolic acidosis
without GI cause)
- Serum phosphorus
- If low, long
bone films
- Serum uric acid
- Urinalysis
- Urine Ca/Cr
ratio
- Urine AA screen
- Renal ultrasound
May consider:
- Urine culture
- Urine electrolytes
and phosphorus
- Urine culture
Acute Kidney Injury
DEFINITION
á
Acute
fall in GFR, which can be indicated by a rise in serum creatinine. Severe AKI
requiring renal replacement therapy is considered acute renal failure (ARF)
á
Most often presents as oliguria/anuria but can
present with normal or increased UOP
o
Oliguria: <0.5 cc/kg/day UOP for infants or
<500 cc/m2/day UOP for older child
o
Anuria: zero urine output
CLASSIFICATION
á
Pre-renal:
hypoperfusion of kidneys due to decreased effective circulating blood
volume
á
Intrinsic
renal: pathology within the kidney leading to decreased function
á
Post-renal:
distal urinary tract obstruction causing back-pressure and decreased
function
Urinary Indices to Classify ARF
|
Classification |
Urine OSM |
Urine NA |
FENa%* |
|
Pre-renal |
>500 >350 (newborn) |
<20 |
<1% <2.5%(Newborn) |
|
Renal |
<350 |
>40 |
>2.5% |
|
Post-renal |
>350 |
>60 |
|
*FENa% = (UNa)(PCr)/(PNa)(UCr)x100%
ETIOLOGY and LAB EVALUATION
Pre-Renal Disease
|
Etiology |
Lab Findings |
|
á Hypovolemia o Dehydration o Hemorrhage o DI o Insensible losses (burns) o 3rd space losses (sepsis, capillary leak, nephrotic) á Hyper/normovolemia o CHF o Cardiac tamponade o
Hepatorenal syndrome |
á FENa <1% or <2.5% in neonates á BUN/Cr ratio elevated á Uosm >400 á
UNa < 10-20 |
Intrinsic Renal
Disease
|
Etiology |
Lab
Findings |
|
Acute Tubular Necrosis (Pre-renal AKI progresses
to ischemic injury, cell death) |
á U/A: protein, WBCs, granular casts |
|
Nephrotoxic AKI/ARF (aminoglycosides,
acyclovir, NSAIDS, IV contrast, chemotherapy, amphotericin B |
á Same as ATN |
|
Exogenous toxins (ethylene
glycol, methanol, heavy metals) |
á Anion gap metabolic acidosis á Hematuria á Ethylene glycol: calcium oxalate crystals |
|
Endogenous toxins (myoglobinuria,
hemoglobinuria) |
á Metabolic acidosis á Heme+ urine without RBC á Elevated CPK |
|
Acute glomerulonephritis (APSGN, IgA nephropathy,
SLE, HSP, MPGN, ANCA vasculitides) |
á Hematuria (may be gross) á Proteinuria, RBC and/or WBC casts á Low C3, C4: SLE, APSGN, MPGN á ANCA: WegenerÕs (C), GoodpastureÕs (P) á +ANA: SLE |
|
Acute interstitial nephritis (penicillins,
NSAIDs, sulfa, rifampin, lasix, cimetidine) *can be post-infectious or idiopathic |
á Urine eosinophils á Urine WBC casts á Serum eosinophilia |
|
Vascular disease (HUS, renal artery or vein
thrombosis, cortical thrombosis ˆ necrosis) |
á Hemolytic anemia (low Hb, high bili, RBC fragments
on smear) á Thrombocytopenia á Hematuria/proteinuria |
|
Nephropathy of malignancy (ALL, B-cell lymphoma) |
á High: K, phos, uric acid á Low: calcium |
Post-Renal
(Obstruction)
|
Etiology |
Lab/Imaging
Findings |
|
Bladder outlet obstruction (posterior urethral valves) Ureteropelvic junction
obstruction Ureterovesicular junction
obstruction |
Hydronephrosis Type IV RTA |
EVALUATION
- First tier:
- Urinalysis and culture
- Urine osmolality, creatinine, and sodium
- CBC
- CMP
- Magnesium and phosphorous
- Renal ultrasound or other imaging study
- Pending first-tier findings:
- Renal biopsy in certain cases
- CPK, urine myoglobin, C3, C4, ASO, ANA
MANAGEMENT
- Remove any potentially offending agent
- NSAID, antibiotic, acyclovir, amphotericin, furosemide
- Evaluate fluid balance and treat based on volume status
- Hypovolemic: 10-20cc/kg bolus to start, monitor UOP and continue accordingly
- Euvolemic: modify maintenance fluids based on UOP
- Oliguric: use 1/3 of maintenance rate to replace insensible losses + replace UOP cc for cc
- Polyuric: start maintenance, monitor UOP and replace cc for cc
- Hypervolemic: start with 1 mg/kg furosemide (max 40 mg), watch UOP, continue accordingly
- Continue to monitor strict IÕs and OÕs, weights (daily or BID), vital signs, capillary
refill, skin turgor, BMP. When these indicate a change in clinical or
volume status, modify fluid orders accordingly!
- Watch for polyuric recovery phase
after oliguric AKI!
- Modify fluids based on electrolytes
(monitor daily)
RENAL REPLACEMENT THERAPY
Indications
- AEIOU mnemonic:
- Anuria
- Electrolytes (dangerous hyperkalemia, refractory acidosis)
- Ingestion (salicylates, toxic alcohols)
- Overload (hypervolemia causing pulmonary edema, CHF)
- Uremia (symptomatic, with AMS)
- Varies based on:
- ChildÕs age, cause of ARF, rapidity of onset
Modalities
- Hemodialysis: aggressive solute
and water removal over limited period of time by passing blood through
artificial filter with countercurrent dialysate flow.
- Advantages:
rapid correction of metabolic disturbances. Treatment of choice for toxin
removal.
- Disadvantages:
large venous access required, difficult if hemodynamically unstable.
- Peritoneal Dialysis: solute and water exchange from peritoneal capillaries into dialysate instilled into the peritoneal cavity. Ultrafiltration is driven by osmotic pressure gradient generated by dextrose.
- Advantages: relatively easy to perform, vascular access not required, does not require hemodynamic stability.
- Disadvantages: slower correction of metabolic disturbances, risk of peritonitis, less control.
- CRRT: continuous more gentle removal of solute and water by passing blood through artificial filter +/- countercurrent dialysate flow. Used in critical illness.
- Advantages: tighter control of chemistry, safe for hemodynamically unstable patients.
- Disadvantage: requires sedated patient and vascular access.
Hematuria
DEFINITION
Hematuria is defined as 5 or more red blood cells per high
power field on a spun urine sample on at least 2 urine samples a week apart
á
Positive blood on a
dip does not equal hematuria. You must do a micro to look for RBCs.
á
A urine dip is only
helpful if it is negative for blood.
4-6% of
asymptomatic school age children will have hematuria on a single specimen. The majority are asymptomatic isolated hematuria, most of which
are benign.
CLASSIFICATION
- Isolated: RBCs on UA but
otherwise, UA, history (including pertinent FH), physical exam (including
growth, BP) entirely normal.
- Non-isolated: RBC on UA with any other
abnormality
- Microscopic: RBC on UA but
normal-appearing urine
- Gross: visibly red/pink or brown
urine that has RBCs on UA when
tested
- Factitious: visibly red/pink or
brown urine that has no RBCs on UA
- Heme (+) on dip: myoglobinuria,
hemoglobinuria
- Heme (-) on dip: other ingestion
such as beets, rifampin, other medications; contamination of cath
specimen with iodine
- Dips for heme have a high
false-positive rate. Consider this in a well child with a positive dip
- Symptomatic- symptoms of urinary
tract/renal pathology such as UTI, rheum, stones, vasculitis, etc
- Functional- Hematuria due to
strenuous exercise, fever, dehydration. Should resolve when circumstances
normalize.
PERTINENT HISTORICAL FACTS
- HPI
- Recent
infection –
- URI, strep, impetigo (for APSGN)
- Diarrhea
(for HUS)
- Urinary
symptoms – dysuria, frequency, urgency, gross hematuria, clots
(UTI)
- Abdominal/flank
pain (stones)
- Arthralgia,
rash, easy bleeding/bruising (rheumatologic)
- Recent
trauma
- Pattern
of hematuria (at end of void in male may be meatal stenosis)
- PMH:
- Birth
history: asphyxia, umbilical vessel catheterization
- History
of HSP
- Chronic
illnesses,
medications
- Recurrent
UTIs
- Sickle
cell disease/trait (papillary necrosis)
- Family history
- Hematuria
- Hearing
loss
- Renal
failure
- Stones
- Cystic
kidney disease
- HTN
- Lupus
- Sickle
cell disease
- Bleeding
disorders
PHYSCIAL EXAM
Complete exam with special
attention to the following:
- Growth
parameters, blood pressure
- Dysmorphic
features
- External ear
anomalies
- Signs of fluid
overload- edema, ascites, rales, pleural rub, gallop
- Abdominal exam-
masses, HSM, pain
- Skin- rashes,
petechiae, purpura
- GU exam –
trauma, rash, adhesions, small meatus
ETIOLOGIES OF HEMATURIA
Glomerular Non-glomerular renal Non-renal
Benign familial Hypercalciuria Stones*
Exercise induced Pyelonephritis Cystitis/prostatitis*
Post-infectious GN* Sickle
cell disease* Foreign
body*
IgA nephropathy* Polycystic
kidney Bladder
tumors*
HSP Reflux
nephropathy AV
malformation
Alport syndrome* Renal
tumor* Hydronephrosis
SLE Renal
Vein thrombosis Perineal
irritation/trauma*
Membranoproliferative
Renovascular HTN
UPJ obstruction
GN,FSGS,MCNS
Abdominal trauma*
Nutcracker syndrome
HUS
* these are more likely causes if there is gross hematuria
LABORATORY EVALUATION
Depends on microscopic v gross, isolated or not,
symptomatic or not
á Asymptomatic isolated microscopic
hematuria
o
Full physical exam with BP and UA weekly x2 to confirm findings
o
If truly asymptomatic and isolated, normal exam and BP, monitor q3-6
months
o
Send Ca:Cr ratio, test parentsÕ urine when able
(benign familial aka thin basement membrane disease)
o
If any abnormality on exam or UA develops, see Ònon-isolatedÓ below
á Non-isolated asymptomatic
microscopic hematuria
o
Urine protein:creatinine ratio if dip shows
protein. Consider 24 hr urine.
¤ If abnormal, refer to nephrology
due to high likelihood of renal disease
¤ If normal, repeat exam, BP, UA in
2-3 weeks
á If hematuria and proteinuria are
resolved, no follow-up needed
á If isolated microscopic hematuria
persists, follow q3-6 months
á If persistent hematuria and
proteinuria, refer to nephrology
¤ Further w/u likely to include:
BMP, albumin, C3, C4, ASO, CBC, renal US, other tests as indicated by history
and these studies
á Symptomatic microscopic hematuria
o
Evaluation based on symptoms – examples of pertinent questions
above
á Gross hematuria
o
Most common causes: UTI, trauma, perineal irritation, kidney stones,
glomerulonephritis
¤ If symptoms, evaluate based on
symptoms, treat accordingly
á In UTI with gross hematuria,
repeat UA after treatment to look for RBC
¤ If no treatable or self-limiting
cause identified, refer to nephrology
o
Initial work-up:
¤ CBC, BMP + albumin (or renal
panel), C3, C4, ASO titer, urine Ca:Cr ratio, renal US
to start
REFERENCE: LAB VALUES
Ca to Cr ratio normal values:
- </= 0.2 ( 7 yrs and older)
- </= 0.4 (19
mos to 6 yrs)
- </= 0.6 (7 to
18 mos)
- </= 0.8
(under 7 mos)
Protein:Creatinine ratio normal
values:
á
</= 0.2 for children
>2 years
á
</= 0.5 for
children <2 years
Proteinuria
DEFINITION
á
>100 mg/m2/day
in children
á
>300 mg/m2/day
in neonates
MEASUREMENT OF
PROTEINURIA - METHODS
- Dipstick
- Trace (10-20mg/dl)
- + 1
(30 mg/dl)
- +
2
(100 mg/dl)
- +
3
(300 mg/dl)
- +
4
(1000 mg/dl)
- Random urine
protein:creatinine ratio
- 24 hour urine
collection
- Fractionated 24
hour urine (night-time and first-morning voids separated from daytime)
- Serum albumin
– if low, there is significant protein loss
DETERMINING IF PROTEINURIA IS SIGNIFICANT
- Dipstick
- ³ 1+ if urine SG ² 1.015 or 2+ if
urine SG > 1.015
- False
positive dipstick possible if urine is concentrated or if pH >8
- False
negative dipstick possible if urine very dilute
- Pro/Cr
- > 0.5 for age 6 mos to 2yr
- > 0.2 for age > 2yrs
- 24 hr urine
- > 100 mg/m2/day
CLASSIFICATION
á Functional Proteinuria – induced by other circumstances, so usually
transient.
o Fever, hypovolemia, stress, exercise, pregnancy, seizures,
CHF
á
Isolated
Proteinuria
o
Lack of associated
signs or symptoms such as casts hematuria, HTN, renal insufficiency, or growth
failure. Negative history.
á
Non-isolated Proteinuria
o
Proteinuria with other
abnormalities on UA or exam, or concerning history. Much more likely to be
pathologic.
ETIOLOGY
á Orthostatic (BOP) – can be
fixed or transient.
o
Proteinuria when upright but not when supine. First AM void will be
negative.
á Glomerular
o
Primary Nephrotic syndromes
¤ Minimal change disease
¤ Congenital nephrotic syndrome
¤ FSGS
o
Immune Complex Glomerulonephritis
¤ Post-infectious GN
¤ MPGN
¤ SLE
¤ Membranous
¤ IgA GN/HSP
¤ Anti-GBM disease
¤ WegenerÕs
o
Abnormal basement membrane composition
¤ DM
¤ FSGS
¤ Alport syndrome
á Tubulointerstitial
o
Primary
¤ Fanconi syndrome – generalized proximal
tubule dysfunction
á Glucose, AA, phos in urine. Low
serum phos, normal glucose
á Assoc w/ mitochondrial disease,
DentÕs disease, Lowe syndrome, cystinosis
¤ PKD
o
Secondary
¤ ATN – from toxic or ischemic
injury
¤ Pyelonephritis
¤ Interstitial nephritis
¤ Obstructive or reflux nephropathy
¤ Heavy metal poisoning
LABORATORY EVALUATION
á Phase I
o
Complete H&P with
BP, growth parameters
o
First AM urine for UA
with micro, Pro/Cr ratio, IF symptomatic ˆ urine cx
o If above
consistent with orthostatic proteinuria, no further evaluation needed. Follow
with yearly first AM urine for U/A and Pro/Cr ratio
á Phase II – if initial
evaluation abnormal
o
CMP – shows
kidney function (Cr, acidosis, K level), albumin (is protein loss significant?)
o
CBC – shows
anemia (anemia of chronic disease suggests kidney disease)
o
C3,C4,
ANA, ASO – may help classify glomerulonephritis
o
RUS –
obstruction, scarring, size, echogenicity, cystic disease all detectable
o
24 hr urine collection
for protein and creatinine
á Phase III
o
Special testing as indicated. May need renal biopsy.
COMMON CONDITIONS
- (Benign) Orthostatic Proteinuria
- Patient
spills protein when upright but not when recumbent
- Diagnosis
in 50-60% of otherwise healthy kids with proteinuria (primarily
adolescents)
- Usually
< 1000 mg total protein in 24 hrs
- Transient
vs. fixed- both have benign clinical course
- Follow
yearly with first AM urine for U/A and protein:Creatinine
ratio
á Nephrotic syndrome
o Defined as massive proteinuria,
low albumin, edema
¤ Elevated cholesterol, TG
associated but not required
o A constellation of findings, not
a diagnosis. Causes include:
¤ Minimal change disease (most
common)
á Usual course: remission within
2-4 weeks, may take up to 8 weeks
á Relapse is common (60%). Up to
4/year is WNL.
á Consider other cause if:
o Child <1 year of age
o HTN, hematuria, or renal
insufficiency
o Not responsive to initial steroid
course
o Frequently relapsing or
steroid-dependent
o These patients need a biopsy
¤ Other causes:
á FSGS
á Congenital nephrotic syndrome
(usually present at <6 mo)
o Initial treatment:
¤ Prednisone 1 mg/kg/dose BID (max
40 mg BID) for 6 weeks, then every other day for 6 weeks with taper
¤ Low sodium diet (2g/day)
¤ NO fluid restriction
o Complications
¤ Infection: antibody proteins are
lost in urine
á Particularly encapsulated
organisms (s. pneumo)
á Peritonitis due to ascites is
classic
á Any fever needs urgent evaluation. If no source, may require cultures,
antibiotics, and observation
¤ Thrombosis: AT-III lost in urine ˆ thrombophilic state
¤ Symptomatic edema: give 25%
albumin (0.5-1 mg/kg) followed by lasix (1 mg/kg, max 40 mg)
á Pulmonary edema with respiratory
compromise
á Extreme, painful GU edema
á Taut, painful ascites
Gastrointestinal
Gastrointestinal Hemorrhage
CONFIRMATION OF BLEEDING
Mimickers of GI bleeding:
á Hematemesis: red food dye or coloring
á Hematochezia: food coloring, red juice/drink, beets, cefdinir, amoxicillin w/ flavoring
á Melena: iron supplement, bismuth (Pepto-bismol), spinach
o False + hemoccult with red meat, iron-rich vegetables
LOCALIZATION OF BLEED
The following characteristics help establish the most likely source:
- Hematemesis: Vomiting of bright, red blood (BRB) or coffee grounds suggests bleeding proximal to ligament of Treitz (distal duodenum)
- Melena: black, tarry stools. Suggests bleeding proximal to the ileocecal valve, significant blood loss (>50-100ml/24hours)
- Hematochezia: BRB or dark, red blood in stools suggests bleeding in the ileum or colon
- Blood streaks on the outside of stool suggests origin as anal canal or rectum
- History of recent epistaxis, coughing, etc., may help localize bleeding to systems other than the GI tract
- In a newborn or breastfeeding infant, consider swallowed maternal blood (Apt test)
ETIOLOGIES OF UPPER GI BLEEDS
á
Duodenal/Gastric ulcer, gastritis:
o
H. pylori, NSAID use,
immune compromise, ICU patients (stress ulcers)
á
Esophagitis:
o
Erosive, herpetic, eosinophilic, candidal
esophagitis; hiatal hernia, GERD
á
Esophageal varices:
o
end stage liver disease
w/ portal HTN, portal vein thrombosis
á
Mallory-Weiss tears:
o
acute vomiting
á
AV malformations
á
Coagulopathy:
o
Liver failure, drugs, DIC from sepsis,
hypersplenism, Vit K deficiency
á
Trauma:
o
sharp ingested FB,
abdominal trauma
á
Milk Protein intolerance
á
Henoch-Schonlein Purpura
ETIOLOGIES OF LOWER GI BLEEDS
á Colitis:
o Infants: milk protein intolerance, Hirschsprung disease, infectious colitis, NEC
o Toddlers: milk protein intolerance, infectious colitis
á Anal fissures: constipation
á Prematurity/LBW: malnutrition, Vit K deficiency, liver disease
á Infectious colitis:
o Salmonella, shigella, E. Coli O157:H7, campylobacter, yersinia, CMV, C. diff, amebiasis
á Henoch-Schonlein Purpura: post-viral, due to vasculitis and edema
á MeckelÕs diverticulum: painless, melena or bright red blood
á Coagulopathy
o Acute or chronic liver failure, congenital coagulopathy (hemophilia, Von WillebrandÕs), hypersplenism, DIC
á Polyps
o <5 yrs: usually juvenile retention polyps, isolated and benign
o >5 yrs: usually polyposis sy ndromes, hamartomas, adenomatous polyps
á Malrotation/volvulus (more acute presentation) – can present at any age
á Intussusception – classic in children <2 yrs, Òcurrant jelly stools.Ó
o If older, look for a trigger for intussusceptions
á IBD:
o CrohnÕs, UC. Acute presentation more likely to be UC.
MANAGEMENT
- ABCs:
- Pulse-ox
goal >95% if significant
anemia (less O2 carrying capacity)
- High
HR, low BP, orthostatic symptoms or VS ˆ
NS boluses while Hb pending
- Position
supine if airway permits. Make NPO.
- If
unstable, urgent GI consult, PICU admission
- Initial
labs:
- CBC-d,
retic, type and screen (or type and cross-match if clear need for PRBCs)
- CMP, PT/PTT
- If
prolonged PT, give Vit K.
- Upper
GI bleed
- place NG, send gastric contents for gastroccult. Leave
NG to lo-int suction or vent
- start PPI
- Lower
GI bleed ˆ
rectal exam, hemoccult stool
- Stool
studies if indicated by history: culture/lactoferrin, C. diff toxin
- Consider
PPI
DIAGNOSTIC PROCEDURES - INDICATIONS
Upper GI Bleeds
- Endoscopy is the procedure of choice. Most accurate when done within 24-48hours of the active bleed.
- Abdominal Ultrasound with doppler flow is helpful when considering portal hypertension or hepatobiliary lesions
Lower GI Bleeds
- Colonoscopy/Sigmoidoscopy: may be difficult in the case of active bleeding. Good for biopsy and diagnosis/treatment of polyps.
- Air Contrast Enema: study of choice when intussusception is suspected. May be diagnostic and therapeutic.
- Scintigraphy Scan (Tagged RBC scan): useful for occult, active bleeding, can detect bleeding at rates as low as 5 mL/hr
- MeckelÕs Scan: technetium pertechnetate concentrates in areas of gastric mucosa – shows ectopic tissue.
- Barium Enema: NO role in lower GI bleeds.
- MRA/CTA: if bleeding persists
Gastroesophageal Reflux Disease
DEFINITIONS
- Gastroesophageal reflux (GER): physiologic in most infants. Self-limited, benign
- Gastroesophageal reflux disease (GERD): reflux associated with symptoms or complications
- Warning signs (suggestive of non-GER diagnosis):
- bilious/forceful emesis
- GI bleeding, diarrhea, abdominal distention /tenderness
- onset >6months of age
- hepatosplenomegaly
- macrocephaly, microcephaly, seizures
COMPLICATIONS
- Systemic: Failure to thrive, ALTE, apnea, anemia, irritability
- most often in infants
- GI: Esophagitis, hematemesis, dysphagia, vomiting , stricture
- Respiratory: Stridor, wheezing, chronic cough,
hoarseness, recurrent pneumonia
EVALUATION
- History:
- Is the child thriving? Detailed feeding history, amount/frequency of spit-ups, associated symptoms (see above), interventions tried already
- Exam:
- Growth, HEENT exam (anomalies, stridor/stertor, pharyngeal irritation)
- Any Òred flagsÓ as above
- If the child is thriving, well, all is c/w GER: reassurance, reflux precautions only
- If any concern for true pathology, consider diagnostic tests:
- Diagnostic tests:
- UGI:
- Use to detect anatomic abnormality. Shows through c-loop of duodenum
- This is sufficient to detect intestinal malrotation
- Small bowel follow-through shows rest of small bowel
- Will show reflux of contrast in almost all babies – cannot tell if pathologic
- pH probe:
- placed through nose into esophagus, left in for 24 hrs.
- Detects frequency of acidic and non-acidic reflux
- Can be used to correlate acid reflux with clinical signs/symptoms
- Second-line test due to invasive nature
- Endoscopy:
- Second-line. Refer pts refractory to treatment or with normal initial tests.
- Can diagnose complications: stricture, ulcerations, dysplasia, eosinophilic or candidal esophagitis
TREATMENT
- Reflux precautions: the ONLY intervention indicated for simple GER
- Upright posture with feedings
- Frequent burping (every 1 oz)
- Smaller, more frequent feeds but ensure adequate total intake
- Elevate the head of the crib
- Feeding options:
- ÒARÓ formulas with added rice thicken in acidic pH, decrease reflux. Do not use with PPI or H2 blockers.
- Consider formula change if concern for milk protein allergy (hydrolyzed formula)
- Try new formula for at least 2 weeks before deciding on efficacy
- Acid reduction therapy: reduces acidity (and thus pain with reflux) but does not reduce reflux of gastric contents.
- H2 blockers: zantac
- PPI: omeprazole, pantoprazole, esomeprazole
- Prokinetic agents: if significant symptoms while on acid suppression or if evidence of delayed gastric emptying
- Erythromycin
- Bethanechol
- Metoclopramide
- Surface agents: Carafate (not as effective in an alkaline environment)
- Mostly used in older children, not much in infants
- Consider GI referral if symptoms still present after 18months of age or any of the warning signs exist.
Neonatal Hyperbilirubinemia
DIFFERENTIAL DIAGNOSIS
Indirect
á Increased Production of bilirubin
o Hemolytic Disease
¯ Immune-mediated (newborn period)
á Rh alloimmunization, ABO and other blood group incompatibilities
¯ Heritable (beyond the newborn period)
á Red cell membrane defects: Hereditary spherocytosis, elliptocytosis, pyropoikilocytosis, stomatocytosis
á Red cell enzyme deficiencies: G6PD, pyruvate kinase deficiency
á Hemoglobinopathies: alpha or beta thalassemia
á Unstable hemoglobins: Congenital Heinz body hemolytic anemia
o Sepsis
o DIC, consumptive coagulopathy, large hemangiomas
o Extravasation of blood: Hematomas; pulmonary, abdominal, cerebral, occult hemorrhage, cephalohematoma
o Polycythemia
o Macrosomia (common in infants of diabetic mothers)
- Increased Enterohepatic Circulation
- Breastmilk jaundice
- Pyloric stenosis
- Bowel obstruction or ileus
- Decreased Clearance
- Breastfeeding failure jaundice
- Prematurity
- Glucose-6-phosphate dehydrogenase deficiency
- Inborn Errors of Metabolism (may also have direct component)
¯ Galactosemia, Glycogen Storage Disorders
¯ Tyrosinemia
¯ Hypermethioninemia
- Molecular defects
¯ Crigler-Najjar Syndrome
¯ Gilbert Syndrome
- Endocrine
¯ Hypothyroidism
¯ Hypopituitarism
Direct
á Obstructive
o Extrahepatic biliary atresia (do not miss this!)
o Choledochal cyst, annular pancreas, diaphragmatic hernia (right sided)
o Spontaneous perforation of the bile duct
o Mass: stone, tumor
á Hepatocellular
o Idiopathic neonatal hepatitis, prematurity
o
Disorders of the intrahepatic bile ducts
o
Syndromic (Alagille) or Nonsyndromic paucity of
intrahepatic bile ducts
o
Caroli disease: congenital hepatic fibrosis with bile
duct cysts
- Metabolic
disorders
¯
Amino acid metabolism: Tyrosinemia
¯
Lipid metabolism: Gaucher disease, Niemann-Pick disease,
Wolman disease
¯
Carbohydrate Metabolism: Galactosemia, Hereditary fructose
intolerance, Glycogen storage disease
¯
Zellweger syndrome and other peroxisomal
metabolism
¯
Bilirubin transport: Dubin-Johnson syndrome, Rotor syndrome
¯
Mitochondrial disorders: Acyl-carnitine
deficiency
¯
Alpha-1-antitrypsin deficiency
¯
Cystic fibrosis
¯
Neonatal iron storage disease
- Endocrine
¯
Hypothyroidism
¯
Hypopituitarism and septo-optic dysplasia
- Infectious
¯
Sepsis
¯
TORCH infections
¯
Hepatitis B
¯
HIV
- Drugs
and Toxins
¯
TPN causing cholestasis
¯
Medications
¯
Fetal Alcohol syndrome
- Vascular
anomalies
¯
Budd-chiari syndrome
¯
Hepatoendothelioma/hemangioma
- Cardiac
insufficiency and hypoperfusion
- Chromosomal
abnormalities
¯
Trisomy 21 and 18
EVALUATION
- Fractionated
bilirubin: must check this on any baby with transcutaneous reading
indicating possible need for phototherapy or follow-up. (high-intermediate risk)
- Direct
hyperbili = direct bili> 2mg/dL or more than 20% of total. This is always pathologic.
- When
did jaundice appear? Within first
24 hours is always pathologic.
- Work-up
of indirect:
- Maternal
ABO/Rh: if O or Rh-, check babyÕs blood type and DAT (standing order in
mom/baby unit)
- Follow-up
levels based on risk category of Bhutani nomogram
- Consider
DDx above. If infant otherwise well-appearing, no other specific history,
physiologic/breastfeeding jaundice most likely
- Work-up
of direct:
- UA
and urine culture
- CMP,
GGT
- Abdominal
US to evaluate biliary tree (gallbladder present? Ducts visible?)
- If
abnormal, HIDA v. ERCP. GI/surgical consultation.
- Check
neonatal screens (if presentation very early, can ask to expedite them)
- Additional
workup is guided by the historical facts and physical exam, i.e. alpha-1-antitrypsin
level, chromosomes, TORCH titers, Hepatitis panel, etc.
- If clinical jaundice or significant
hyperbili persists, repeat a fractionated bilirubin weekly. Biliary
atresia is progressive and must be caught early.
MANAGEMENT AND PREVENTION
Prevention: Goal is to prevent bilirubin encephalopathy (Kernicterus)
á All newborns discharged <72h after birth should be seen within 2 days of discharge
á Consider risk factors for severe hyperbili when determining follow-up:
o Bilirubin in high-risk zone
o Late prematurity
o Positive DAT, blood group incompatibility
o Sibling who required phototherapy
o Significant cephalohematoma
o Polycythemia (delayed cord clamping, IDM)
o Exclusive breastfeeding
¤ Encourage 8-12 feedings per day, involve lactation consultant if trouble
Treatment
á Direct hyperbili: treat underlying cause
o Do not use phototherapy – can cause bronze baby syndrome and blistering
á Indirect hyperbili: phototherapy and feeding are key
o Consider ddx above. Physiologic jaundice is most common, but other conditions are possible!
o Use nomogram to determine phototherapy threshold
o Babies may continue to breastfeed, with time limits (30 min every 2 hours, under the lights at all other times)
o Other interventions such as labs, fluids on an individual basis depending on hydration status and how well the baby is feeding
o Discontinue phototherapy when bili <12
o Signs of acute bilirubin encephalopathy = need immediate exchange transfusion
¤ Extreme lethargy or irritability, high-pitched cry, poor suck
o If bili still rises despite phototherapy in isoimmune disease, can use IVIG.
¤ 0.5-1 mg/kg over 2 hours, can repeat in 12 hours.
FIGURE 1:
ESTABLISHING RISK ZONE
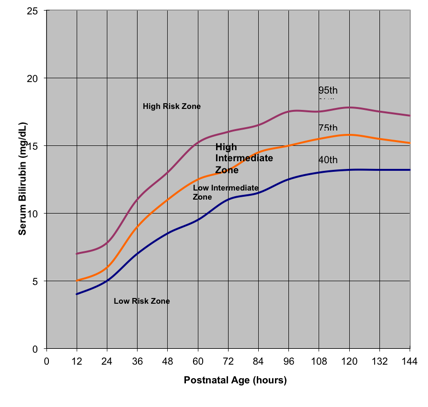
FIGURE 2
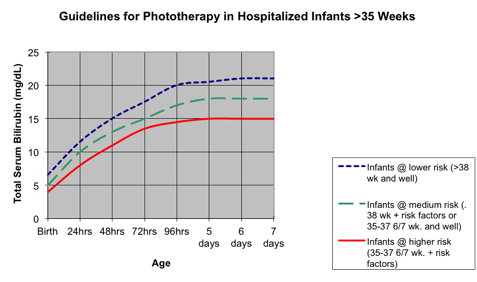
Neurotoxicity
risk factors
á
Isoimmune
hemolytic disease
á
G6PD deficiency
á
Birth asphyxia
á
Significant
lethargy
á
Temperature
instability
á
Sepsis
á
Acidosis
á
Albumin <3
Diarrhea
Differential
Diagnosis
á
Acute:
o
Viral gastroenteritis
o
Bacterial enteritis
o
Other infection: otitis media, pneumonia can
cause loose stools in infant/toddler
o
Antibiotic-associated diarrhea
o
Overfeeding/improper mixing of formula (in
infants, due to hyperosmolar intake. can also be chronic.)
o
Lactase deficiency (often transient,
post-infectious)
o
Serious
conditions that can present with acute diarrhea:
¤
Appendicitis
¤
Intussusception
¤
C diff colitis
¤
Toxic megacolon
¤
HUS
¤
Organophosphate poisoning
á
Chronic:
o
Functional diarrhea (toddlerÕs diarrhea)
o
Post-enteritis syndrome: mucosal damage after
acute gastroenteritis
o
Malabsorption (carbohydrate, protein, or fat)
¤
Mucosal problem (disaccharidase, mucosal
inflammation from IBD)
¤
Lymphangiectasia ˆ protein loss
¤
CF or other pancreatic insufficiency
o
Celiac disease
o
HirschsprungÕs disease
o
IBD
o
Allergic enteropathy (i.e. milk protein
intolerance)
o
Eosinophilic gastroenteritis
o
Short bowel
o
Encopresis/functional constipation (CC is
usually diarrhea)
o
Hyperthyroidism
o
In
immunocompromised patients: bacterial, parasitic organisms
¤
HIV can
present this way
o
Congenital secretory or malabsorptive diarrheas
¤
Severe, present early in infancy
o
Secretory tumors (VIPoma, gastrinoma,
mastocytosis)
Evaluation
á History
o Acute diarrhea:
¤ Bloody stools c/w bacterial infection or more serious causes above
¤ Known exposure or sick contact? Contact w/ pets? Travel?
¤ Associated symptoms, fever
o Chronic diarrhea:
¤ Age of onset
á Neonatal: congenital malabsorptive and secretory syndromres, milk protein intolerance
á Toddlers: toddlersÕ diarrhea, celiac disease
á Teens: IBD
¤ Characteristics of stool
á Blood/mucus: IBD, MPI, chronic infectious diarrhea, C. diff
á Watery: toddlersÕ diarrhea, carbohydrate Malabsorption, celiac
á Greasy/foul-smelling: fat malabsorption
á Small volume incontinence: encopresis
¤ Other medical conditions: immune compromise, hx of abdominal surgery, short bowel syndrome
¤ Growth:
á Failure to thrive or weight loss: malabsorption, IBD, hyperthyroidism
á Weight loss in teens: consider laxative abuse
¤ Recurrent infections? Unexplained fevers?
á Exam
o Very sick v. mildly sick?
o Complete exam focused by history
á Labs
o Acute diarrhea:
¤ Fecal lactoferrin: marker of WBC activity, should be + in infectious or inflammatory cause
á If negative, no need to culture. If positive, culture if a known organism will change management
á If you know you need to obtain a culture, do not order this
á Breastfeeding: lactoferrin WILL BE (+). Order fecal WBC instead
¤ Giardia antigen by EIA, O&P based on history
o Chronic diarrhea: individualized based on history and DDx being considered
¤ First: exclude toddlersÕ diarrhea, celiac, giardia (if any pertinent history)
á ToddlersÕ diarrhea: history
á Giardiasis: Giardia antigen test
á Celiac disease: TTG, total IgA
á Check hemoccult
á Fecal lactoferrin
¤ Watery diarrhea: secretory v osmotic
á NPO for 24 hrs.
o If diarrhea continues in fasting, it is secretory
o If diarrhea resolves with fating, it is osmotic
á stool osmolal gap: 290 – 2(stool Na + stool K)
o gap <50, pH >6 likely secretory
o >125, pH <5.5 likely osmotic
á Stool reducing substances: if positive, likely carb Malabsorption
o Reducing sugars: lactose, glucose, fructose (NOT sucrose)
¤ Other tests to consider for specific conditions:
á Infectious/inflammatory: fecal lactoferrin or culture
á Protein malabsorption: fecal alpha-1-antitrypsin
á Fat malabsorption: fecal elastase (marker of exocrine pancreatic function)
Endocrine
Diabetes Mellitus
DEFINITION
- Fasting glucose >126 mg/dL
- Random glucose >200 mg/dL PLUS symptoms
- Hb A1c > 6.5
- DKA defined as Glucose >250 mg/dL and pH <7.25 or HCO3 <15 mmol/L and presence of urinary or serum ketones
EVALUATION
History
á
Polyuria, polydipsia, nocturia, weight loss
á
Polyphagia (often not present in children and
new onset Type I diabetes with ketosis)
á
Vomiting, headache, abdominal pain
á
If known diabetic:
o
insulin dose and
regimen (pump v shots; basal, correction, I:C) and time of last insulin.
o
Known trigger: viral illness, vomiting, forgot
insulin, etc.
o
If on a pump: last site change and if any problems
occurring
á New onset DM: Assess for symptoms or FH of autoimmune disease (e.g. DM, thyroid, vitiligo, rheumatoid arthritis, SLE, celiac disease, MS, etc.)
Physical
á
ABCs, neuro status
o
DKA pts – signs of elevated ICP?
á
Assess hydration status
á
Growth parameters, BMI
o
Obese – consider type 2 DM, w/u below
o
Short stature: consider thyroid, adrenal
problems, celiac dz
á
Thyroid exam
á
Skin:
Acanthosis nigricans, striae, vitiligo
á
Pubertal status
Initial Laboratory Evaluation
á
Fingerstick blood glucose immediately
á
Stat BMP and urinalysis (dipstick okay). *bicarb <15 is cutoff for PICU
á
ABG/CBG if very ill-appearing, considering PICU
á
New onset diabetic:
o
HbA1C, GAD 65 Ab, ICA 512 (IA-2) Ab, Insulin
Autoantibodies
o
When out
of DKA: TSH, Total T4, anti-peroxidase and anti-thyroglobulin antibodies
o
Test for celiac disease only if symptomatic (tissue transglutaminase IgA with concurrent
total IgA for validation)
á
If obese:
insulin level or C-peptide level (must be drawn prior to exogenous
insulin administration).
o
Lipids and urine for microalbumin should be
checked as outpatient
á
Notify endocrinologist on call.
o Full consult for all new onset patients; at team or endocrineÕs discretion if known diabetic
á New onset patients: consult diabetes educator and nutrition
THERAPY
- Usually start insulin at 1unit/kg/day, less than age 5 start 0.6-0.8 units/kg/day.
- Basal-Bolus Insulin regimen:
¤ Long acting ÒbasalÓ insulin (Lantus or Levemir): 40-50% of total daily dose given at bedtime
¤ For new onset patient, start with 40%
¤ Short-acting ÒbolusÓ insulin (novolog, humalog, regular insulin)
¤ The insulin:carb ratio covers for carbohydrates consumed.
v Divide 500/total daily dose of insulin: 50 kg kid ˆ 500/50 = 10, so I:C = 1:10. One unit of insulin per 10g carbohydrate.
¤ Correction formula covers for a high blood sugar (checked AC, HS):
v CF = (BS-target glucose)/sensitivity factor
v The target glucose is usually 120. For children <5 years, 150.
v Sensitivity factor:
¤ If insulin sensitive divide 1800 by total daily dose of insulin.
¤ If insulin resistant divide 1500 by total daily dose of insulin.
¤ Insulin sensitivity/resistance determined by clinical judgment
- Alternate insulin regimens may be used at the discretion of Endocrinology
INPATIENT MANAGEMENT – GENERAL FLOOR
á
Diet should be ÒNCS Diabetic DietÓ – NCS =
no concentrated sweets
á Check glucose Q2hours until ketones 20 or less (trace). Then check AC, HS, 2 AM (may not need 2 AM check in known diabetic)
á Check glucose ˆ patient eats ˆ calculate insulin to cover carbs (I:C ratio) and correction for pre-meal glucose (CF) ˆ total this up and give one injection.
á Insulin to cover carbs can be given whenever patient eats
á Correction insulin for high blood sugar cannot be given more frequently than Q2 hrs – this can cause insulin stacking and hypoglycemia
á Check urine ketones for all BS>240
á Ketone management: check ketones Q void until clear, check glucose Q2 hrs.
o If patient is asleep and on IV fluids, continue fluids
o If patient is not on IV fluids, have patient drink:
¤ BS >300: age in oz of sugar-free fluid
¤ BS 180-300: age in oz of 1:1 ratio sugar-containing and sugar-free
¤ BS < 180: age in oz of sugar-containing fluid (juice)
o For all patients, correct blood sugar and cover for carbs consumed if applicable
¤ +1 extra unit if 5-12 years
¤ +2 extra units if >12 years
HYPOGLYCEMIA IN
THE DIABETIC
- If
awake and alert, give 15 grams of carbs and reassess in 15 minutes.
- If
alert but cannot tolerate PO intake, give 5 mL/kg bolus of 10% dextrose
- If
not alert, give Glucagon kit IM/SQ (available on the floor). Watch for emesis. Turn on side.
DKA MANAGEMENT -
PICU
Initial Management
á First, ABCs!
á Bolus 10-20cc/kg NS over 1hour, reassess after first bolus, re-check BMP and POC gluc
- Do NOT give insulin bolus. Anticipate starting insulin after fluid bolus.
- PICU admission required for altered level of consciousness, need for insulin drip
- Insulin drip for bicarb <15 or at teamÕs discretion (extremely high glucose, very young patient, etc)
Nursing Orders
- Cumulative
I&Os
- Vital
signs with neuro checks q1hour, POC glucose Q1 hr
Fluid and Insulin Management: 3-bag method
- Assume about 10% dehydration for DKA admission
- Rehydrate (deficit + maintenance) over 48 hrs – usually approx. 2x MIVF rate
- Use ½ or ¾ NS to limit chloride load (can worsen acidosis)
- 3 bags:
- Regular insulin
- ½ or ¾ NS + 15 mEq/L K-phos + 15 mEq/L K-acetate
- D10% with ½ or ¾ NS + 15 mEq/L K-phos + 15 mEq/L K-acetate
- (Add K, phos to fluids anticipating drops with correction of acidosis)
- Method:
á
Began insulin infusion at
0.05units/kg/hour. Use Regular
insulin.
á
Start fluids with NO dextrose (D10 bag is off)
á
When glucose 250-300, run dextrose-free fluids
at ½ of total rate, start D10% fluids at ½ of total rate ˆ
patient receives D5%
á
When glucose 200 or less, run d10% fluids at
full rate, stop dextrose-free fluids.
á
Goal is blood sugar drop of 75-100 mg/dL per
hour
o
If dropping too fast,
increase dextrose and keep insulin drip going – insulin is needed to
correct acidosis.
á
If transition is anticipated by morning, give
Lantus HS per patientÕs known regimen or as calculated above for new onset
patient
Monitoring
- Q1hour: Bedside glucose, VS, neuro checks,
and cumulative I&Os
- Q4hour: BMP, Mg, Phos
- Ketones will be positive in DKA. Start checking urine ketones when patient is close to transition off the drip. Ketone management post-DKA above.
Transition to Maintenance Therapy
- DKA
resolved when bicarb >15, anion gap closed, able to tolerate PO
- If
basal insulin was given HS before transition, can stop drip any time
- Have
patient eat, give correction insulin (CF, I:C),
stop insulin drip AND dextrose-containing fluids
- If
basal insulin has not yet been given: give full dose at time of
transition, wait 30 min, then stop drip AND dextrose-containing
fluids.
- If
Lantus given in the AM, push the time of administration back over several
days to
get back to usual HS schedule (lunchtime the next day, then late
afternoon, then HS)
- If transitioning at night or if ketones still present, continue IV fluids with NO dextrose.
- Consider NPH as an option if transitioning in the morning-consult Pediatric Endocrinology for recommendations.
INSULIN
PREPARATIONS
- Rapid: 5-15minute onset. Peak 1-2hours. E.g. lispro (Humalog), Aspart (NovoLog), Glulisine (Apidra). All insulin pumps use rapid acting insulin. Basal bolus regimens use rapid acting insulin in addition to a once a day long acting insulin.
- Short: 30 minute onset. Peak 2-4 hours. Regular (Humulin R/Novolin R)
- Intermediate: 2 hour onset. Peak 6-10 hours. Duration 10-18 hours. NPH
(Humulin N/Novolin N)
- Long: 1-2 hour onset with 24 hour duration (peakless). E.g. Glargine (Lantus), Detemir (Levemir). Often used with basal-bolus regimen.
Hypoglycemia
DEFINITION
Pathologic hypoglycemia: serum glucose (not ÒfingerstickÓ) < 50mg/dl, regardless of age. Symptoms: vary by age.
á Infants: jitteriness, hypotonia, apnea, tachypnea, lethargy, poor feeding, hypothermia
á Children/adolescents:
o Neuroglycopenic symptoms: pallor, confusion, weakness, altered mental status, irritability, seizure, coma
o Autonomic response: sweating, tachycardia, palpitation, tremor, paresthesia
ETIOLOGY
- Hypoglycemia in the neonate: Infant of Diabetic Mother, Glycogen Storage Disorder, Hypopituitarism, Peripartum stress, Small for Gestation Age, Prematurity, Inborn error of Metabolism, Hydrops Fetalis, Beckwith-Wiedemann Syndrome
- Hypoglycemia with ketosis:
- Ketotic Hypoglycemia: most common etiology.
- Age 18mo-5years, usually thin. Male predominance. Unknown etiology.
- Prevention with frequent complex carbs and protein (bedtime snack).
- May need to teach families to monitor for ketones during illness.
- Sepsis or other hypermetabolic states
- Dumping syndrome (usually tube-fed or short bowel patient)
- Primary, central, or iatrogenic adrenal insufficiency, GH deficiency
- Organic acidemias
- Ingestion: alcohol, salicylates, beta-blockers, sulfonylureas
- Hypoglycemia without ketosis:
- Neonate: Hyperinsulinism – IDM, congenital hyperinsulinism, exogenous insulin, insulinoma
- Fatty acid oxidation defects (MCAD, carnitine disorders)
- Glycogen storage diseases (except type 0)-hepatomegaly
- Defects in carbohydrate metabolism: Hereditary fructose intolerance, galactosemia
- Pancreatic adenoma-later in childhood
EVALUATION
- Historical
Facts: prenatal history,
prematurity, SGA, diet (?starvation), new foods,
medications, developmental delay, FH, social history (exposure to alcohol,
steroids, sulfonylureas, insulin)
- Plot on growth curve: Short stature concerning for endocrine/IEM etiology
- Physical Exam: Organomegaly (IEM/GSD), hyperpigmentation (primary adrenal), and look for midline defects-hypopituitarism (i.e. microphallus, small optic nerves, cleft lip/palate, central incisor)
- Must collect Òcritical sampleÓ while the patient is hypoglycemic
CRITICAL SAMPLE
á Serum Glucose (confirmation of fingerstick)
á Red Top (3-5cc, iced) for *Cortisol*, *Growth Hormone*, Insulin and/or C-peptide
o Insulin AND C-peptide (if concern for exogenous insulin)
o Insulin >2-3 micro-IU/mL or insulin:glucose > 0.25 ˆ hyperinsulin state
á Red Top (3-5cc) refrigerate for possible later use
o Consider: Ammonia, serum amino acids, hydroxybutarate, lactate, free fatty acids
á Urinalysis (ketones/reducing substances)
o + reducing substances in galactosemia, hereditary fructose intolerance
á Other lab tests: CMP, Ammonia (need not be done at time of hypoglycemia)
o Acidosis and elevated ammonia suggest IEM
á If symptoms recurrent or concern for IEM
o serum amino acids, urine organic acids, plasma acylglycines, free/total carnitine profile (ideally during acute episode but can be done later).
á
*If unable to get enough blood at time of
hypoglycemia, Growth hormone and cortisol can be drawn up to 30 minutes after
hypoglycemia, even if treatment is started*.
TREATMENT
- If patient tolerating PO, give 15g fast-acting glucose, re-check 15 minutes
- If cannot take PO:
- Bolus with 5cc/kg of D10 peripherally or 2cc/kg of D25 centrally
- Begin continuous infusion of D10 with goal glucose infusion rate (GIR) 6-8mg glucose/kg/min See Òquick calculationsÓ for GIR formula
- If >10-15mg glucose/kg/min required, consider hyperinsulinemic state.
- Consult Endocrine
- May need diazoxide (3-8mg/kg/day given TID, 15mg/kg/day given TID for infants), somatostatin, or glucagon.
- Further treatment is guided by suspected underlying pathology.
Adrenal Insufficiency
Adrenal insufficiency:
á Congenital or acquired
á Primary-disorder of adrenal gland
á Secondary-pituitary or hypothalamic issue
When to Suspect Adrenal insufficiency:
- Virilized female neonate/Ambiguous genitalia (CAH)
- Congenital adrenal hypoplasia
- Midline defects (septo-optic dysplasia, hypopituitarism)
- History of recent high-dose steroid use or neonate born to mom with recent steroid use
- Hyperpigmentation, fatigue, weight loss (AddisonÕs disease)
- Other causes:
- Hypothalamic/pituitary tumor, hx cranial irradiation or surgery, head trauma, autoimmune disease (autoimmune polyglandular syndrome), infection (TB, fungal, HIV, CMV, histoplasmosis), sarcoidosis, adrenal hemorrhage (neonatal or post-partum), ketoconazole/fluconazole use use, numerous steroid synthesis defects, adrenoleukodystrophies, Langerhans cell histiocytosis, Wolman disease
Signs/symptoms:
á Primary: hyperpigmented (generalized, extensor surfaces, palmar creases, gingival margins), salt craving, hyponatremia, hyperkalemia, ‡ACTH, ‰Aldosterone
- Adrenal crisis: hypotension (may be postural), mental status changes, or shock/coma
- Non-acute: anorexia, weight loss, malaise, fever, abdominal pain, NVD, dehydration
- Metabolic disturbance:
- Primary: hyponatremia, hyperkalemia, hypoglycemia, hypercalcemia, and acidosis , ‰ Cortisol, ‡ PRA
- Central: may not see Na or K abnormalities, b/c renin/aldo pathway not affected)
EVALUATION OF ADRENAL INSUFFICIENCY (non-emergent)
- BMP,
ACTH, cortisol
- Cortisol
level interpreted in context: time of day, blood glucose, and presenting
symptoms [should be elevated
in a critically ill patient]. If possible, order 8 AM cortisol
with concurrent glucose
- If
electrolyte abnormalities, check aldosterone and renin.
- In
infants, check 17-hydroxyprogesterone
- Cosyntropin stimulation testing can aid in
diagnosis. ACTH and cortisol
should be drawn at baseline.
- To dx adrenal source: Give 250 mcg cosyntropin, check cortisol in 1 hour. <18mcg/dl is abnormal.
- To dx central (pituitary or hypothalamic) source: give 1 mcg, check cortisol at 10 min, 30 min. <18 mcg is abnormal.
- Dexamethasone does not interfere with results
MANAGEMENT OF ADRENAL CRISIS
- Emergent: treat ABCs, life-threatening electrolytes
- Low BP ˆ NS bolus, repeat as needed
- Low glucose ˆ 5cc/kg D10 (or 2 cc/kg D25 if central line), continue as needed
- IVF at 1.5-2 times maintenance
- Solu-Cortef (50-100mg/m2/day) every 6 hours until patient is stable. (Higher doses can be used if necessary to correct hyponatremia or hyperkalemia or consider fludrocortisone).
- Check BMP or, if critical, ABG with electrolytes (faster). Correct hyper-K.
- Identify precipitating condition for adrenal crisis (i.e. infection) and treat appropriately
- Stress dose glucocorticoid (hydrocortisone) required in cases of acute adrenal crisis.
- If stress dose unknown, triple the daily dose of oral hydrocortisone (known pt) or triple the physiologic dose (new onset)
- Physiologic dosing: Hydrocortisone NaSuccinate 10-15mg/m2 BSA/day po
- lower end of the range for hypopituitarism and higher for CAH
- Stress Dosing:
- Critical: Solu-Cortef load 50-100mg/m2 BSA IV bolus then 100mg/m2 BSA/day IV continuous infusion or divided q 6 hours
- Non-critical or at home: triple maintenance dose, PO
- See Quick calculations section for BSA calculation
- When stable (at baseline for 24 hours), the dose should be tapered back to maintenance and changed to po
- Mild hyponatremia may develop as cortisol is required to excrete free water
- Patients with primary adrenal insufficiency require mineralocorticoid:
- Florinef 0.05-0.2mg/day (fludrocortisone)
- If primary vs. central unknown, consider this if hyponatremia persists despite hydrocortisone, if high urine Na or high renin
- If infant; may need to use salt (NaCl) 2-4 meq/kg/day instead of Fludrocortisone until kidneys mature.
BIOEQUIVALENCY OF GLUCOCORTICOIDS
|
Steroid |
Equivalent Dose (mg) |
Relative Glucocorticoid activity |
Relative Mineralocorticoid activity |
Half-life (hrs) |
|
Hydrocortisone |
20 |
1 |
1 |
8-12 |
|
Prednisone |
5 |
4 |
0.8 |
12-36 |
|
Prednisolone |
5 |
4 |
0.8 |
12-36 |
|
Methylprednisolone |
4 |
5 |
0.5 |
12-36 |
|
Fludrocortisone |
n/a |
10 |
125 |
12-36 |
|
Dexamethasone |
0.75 |
30 |
0 |
36-72 |
Diabetes Insipidus
Diagnosis
á Polyuria (5 cc/kg/hr) or history (increased urine output/ excessive number of wet diapers)
o DDx includes: Central DI, nephrogenic DI, cerebral salt wasting, primary polydipsia, diabetes mellitus (check the glucose!)
á Clinical history for DI:
o Central: Hypopituitarism, midline defects, hx HIE or acute head trauma, pituitary surgery, meningitis, infiltrative disease (Langerhans histiocytosis, sarcoidosis), CNS tumor/lesion
o Nephrogenic: most often x-linked defect in V2 receptor gene or AD/AR defect in aquaporin-2 gene
¤ In adults, most common cause is lithium
Lab evaluation
á Urinalysis-what is the Specific Gravity
á Serum Na and Serum osmolality (or calculate from BMP, see Òquick calculationsÓ page)
á Urine osmolality (+/- urine Na)
á Findings:
o High serum Na and dilute urine (urine osm < serum osm) c/w DI
¤ Response to DDAVP determines central vs. nephrogenic
o Low serum Na and low urine osm c/w primary polydipsia
Treatment
á
STRICT
IÕs & OÕs
á Central DI
o If mild, fluid replacement with free water. If using IVFÕs, use 0.45%NaCl or more dilute
¤ If severe, DDAVP (PICU setting)
¤ IV (if acute or cannot take PO meds): depends on weight and age. Start with lowest dose. DonÕt schedule dosing initially.
¤ Check Na Q4-6 hrs
¤ Watch UOP closely – Q1-2 hr. this is an indication for a foley catheter.
¤ Do not re-dose until breakthrough UOP
¤ Dosing and follow-up should be discussed with endocrine.
á Nephrogenic DI
o Treatment depends on etiology.
o Decreased solute (Na) intake: if concentrating ability is fixed, less solute = less diuresis.
o Thiazide diuretics: induces hypovolemia ˆ more proximal salt and water reabsorption ˆ less distal sodium delivery ˆ less diuresis.
o NSAIDs: increase sensitivity to ADH. Especially helpful in BartterÕs syndrome.
Puberty
- Normal ages of onset: boys 9-14, girls 8-13
- Controversial. Some advocate boys age 8, girls age 6-7.
- Earlier on average in African-American children & Hispanic children.
- Premature adrenarche not uncommon in
overweight children.
- Pulsatile secretion of LH and FSH (gonadotropins) ˆ gonadal maturation and production of the sex steroids.
- Random LH and FSH may not be helpful in evaluation of precocious puberty. They are helpful when evaluating delayed or late puberty.
- Best time to measure is morning/fasting
- Clinically, maturation of the hypothalamic-pituitary-adrenal (HPA) axis ˆ adrenarche (pubic/axillary hari, acne) at the same time as maturation of the hypothalamic-pituitary-gonadal (HPG) axis ˆ secondary sexual characteristics.
- Biochemically, adrenal DHEA-S may be measurable before gonadal steroids.
- Girls:
- Thelarche first ˆ adrenarche ˆ menarche
- Peak linear growth rate in height occurs at Tanner II-III.
- Menarche occurs at Tanner IV (~2 years after thelarche).
¯ Signs of virilization: clitoromegaly, hirsuitism, male patterned (temporal) baldness, recalcitrant acne, deepening of the voice
¯ Signs of estrogen: breast tissue, thickened, lighter pink vaginal mucosa, menses, and increased height velocity
- Boys:
- testicular enlargement is the first sign of true puberty ˆ penile lengthening ˆ pubic and axillary hair.
- Peak linear growth rate occurs at Tanner IV. Higher peak velocity and longer duration of linear growth.
- It is important to follow the rate of growth. Early rapid growth is abnormal.
- First evaluation for abnormal puberty/growth: start with bone age.
- Over age 2: XR of left hand/wrist.
- Under age 2: left hemi-skeleton.
- Abnormal if a difference of 2 standard deviations exists (typically >2years).
PRECOCIOUS PUBERTY
Defined as Girls < 8 and Boys < 9
True Puberty (gonadotropin dependent) or Central Precocious Puberty
á Definition: onset of puberty2 SD earlier than population mean (see ages above)
- Normal cascade of events with activation of HPG axis. +/- adrenarche
- Rapid progression is abnormal
- Etiologies include: idiopathic, CNS lesions, non-progressive CNS disorders (CP)
- Girls: most likely idiopathic
- Boys: most likely pathologic
- Workup:
- Tier 1: complete neurologic exam including visual fields, Gender-specific sex steroid (Girls: sensitive estradiol; boys: total testosterone), total T4, TSH, and consider LH, FSH, and DHEA-S
- If any Tier 1 findings concerning for pituitary/hypothalamic source: MRI of brain with contrast and hypothalamic-pituitary cuts
False Puberty (gonadotropin independent, peripheral precocious puberty)
- Does not proceed through normal order of pubertal events.
- Etiology: abnormal sex steroids from gonads/adrenal gland or exogenous (ingested, topical) source.
¯ Rare causes: McCune-Albright syndrome, severe hypothyroidism, βHCG secreting tumors (in boys).
- Premature Pubarche (pubic hair) and/or Adrenarche (pubic and axillary hair) etiologies:
¯ Benign premature adrenarche, simple virilizing/nonclassic congenital adrenal hyperplasia, virlizing drugs/tumors (includes anabolic steroids, creams/lotions).
¯ Benign premature adrenarche: most common cause of early pubarche. Benign elevation of adrenal androgens (DHEA-S). No growth acceleration, advanced bone age, rapid progression, or virilization.
¯
Initial w/u: 17-hydroxyprogesterone, total
testosterone, DHEA-S, and a bone age.
- Premature
Thelarche: Appearance of
breasts prior to age 8. No
evidence of growth acceleration, rapid progression, or other signs of
estrogen exposure. Not uncommon in
girls 18-24 months. 10% progress to true precocious puberty.
¯ If present consider bone age, sensitive estradiol, total T4, and TSH.
¯ If labs abnormal, pelvic ultrasound (for estrogen-producing tumor of ovary)
- Premature menarche: Rare presentation of precocity. If no other evidence of sexual maturation exists, ovarian disease (dominant cyst or malignancy) must be excluded. Rule out foreign body, infection, abuse/trauma, or local neoplasm. Evaluation includes sensitive estradiol, T4, TSH, pelvic ultrasound and bone age.
DELAYED PUBERTY
á Delayed puberty definitions:
o Girls: onset >13 OR no menses by 16 despite secondary characteristics
o Boys: onset >14
á ÒArrestedÓ puberty: menarche occurs 5years after normal thelarche
á Evaluation
- History: chronic illness, anosmia/hyposmia, colored-blindness, signs of hypothyroid, Family history
- Physical Exam: growth, Tanner stage, stigmata of Turner Syndrome or other genetic disorders, complete neurologic exam (includes visual fields; may need to assess olfactory sense or color perception
- Lab:
- First tier: LH, FSH, thyroid functions, and bone age
- Classification:
¯ Hypergonadotropic Hypogonadism (increased LH/FSH): Turner syndrome (most common cause of ovarian failure in girls!), Klinefelter syndrome, Bilateral gonadal failure (traumatic, postinfectious (mumps), galactosemia (poorly controlled esp. in girls), autoimmune, iatrogenic (post-surgical), vanishing testes syndrome
¤ Turner Syndrome:
á Consider karyotype in all short girls with delayed puberty
á May have minimal breast development; menses rare. Adrenarche typically normal.
¯ Normal to low Gonadotropins: Constitutional Delay (very common), Hypothalamic dysfunction, Chronic Illness, Hypopituitarism, Hypothyroid, Hyperprolactinemia, Kallman syndrome (isolated Gonadotropin deficiency)
¤ Constitutional Delay: Pubertal increase in gonadotropins is slow.
á More common in boys. Often FH of Òlate bloomers.Ó
á Evaluation normal except delayed bone age consistent with pubertal stage and height age.
- Amenorrhea with normal pubertal development:
- DDx: pregnancy, Rokitansky syndrome (absent uterus), imperforate hymen
- Also
consider thyroid functions, prolactin, pelvic
ultrasound.
- Polycystic Ovarian Syndrome/Hirsutism:
- Associated with obesity, glucose intolerance, and anovulatory cycles.
- DDx includes late-onset CAH.
- Work up includes free testosterone, 17-hydroxyprogesterone (AM), LH/FSH ratio, prolactin and fasting insulin with glucose, TSH, T4 (free T4 may be superior here). Consider lipids, OGTT, A1c.
- Best treatment is lifestyle changes with weights loss. Rx may include Metformin and/or OCPs.
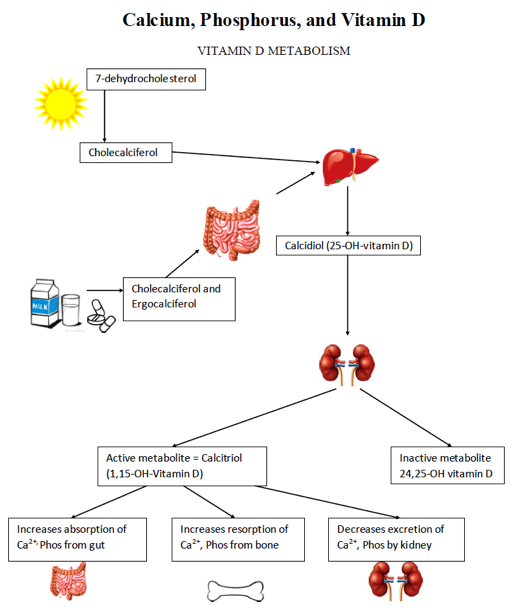
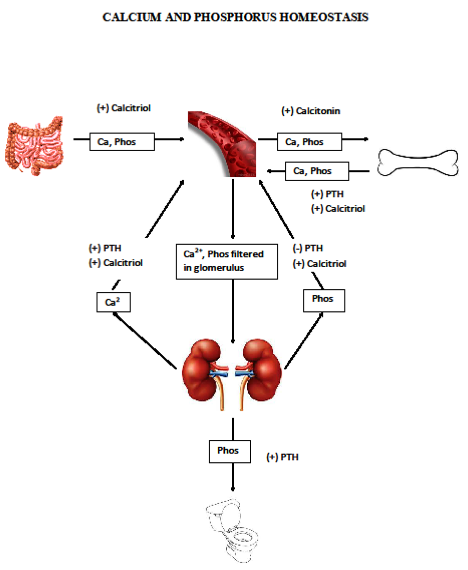
Decreased serum calcium stimulates PTH production ˆ PTH stimulates action of Calcitriol (active Vit D). Both work as above to increase serum calcium while maintaining serum phosphorus. Thus, significant Vitamin D deficiency leads to hypocalcemia and rickets (young children) or osteomalacia (older children).
CAUSES OF HYPOCALCEMIA
![]() Serum
Urine
Serum
Urine
Causes of Hypocalcemia Ca Phos PTH Alk
Phos
25-OHD3 1,
25(OH)2D3 Mg Ca
Vitamin D-deficient ↓↔ ↔↓ ↑ ↑ ↓ * ↔ ↓
Rickets
Vitamin D-dependent
Rickets: type 1 ↓
↓ ↔ ↑ ↑ ↔ ↓ ↔ ↓
Vitamin D-dependent
rickets type II ↓
↓ ↔ ↑ ↑ ↔ ↑ ↔ ↓
Vitamin D
Resistant rickets ↔
↓ ↔ ↑ ↔ ↔↓ ↔ ↓
(hypophosphatemic
rickets)
Hypoparathyroidsim ↓ ↑ ↓ ↔ ↔ ↔ ↓ ↔ ↓
Pseudohypoparathyroidism ↓ ↑
↑ ↔ ↔ ↔↓ ↔ ↓
Rickets of prematurity ↔ ↓ ↔↓ ↑ ↑ ↔ ↔↑ ↔ ?
Renal osteodystrophy ↓ ↑ ↑ ↑ ↔ ↓ ↔ ↓
Calcium-sensing receptor
defect ↓ ↑ ↔
** ↔ ↔ ↔ ↓ ↔ ↑
Mg deficiency ↓ ↔ ** ↔ ↔ ↓ ↔ ↑
?= difficult to interpret owing to different degree of
renal immaturity in preterm infants
*= low
or normal or high
Presentation of
Rickets
á FTT/short stature
á Developmental delay/weakness
á Non-specific MSK complaints
á Seizures/tetany
á Rachitic rosary, widening of wrists and ankles
á X-ray: widening, fraying, cupping of metaphyses, osteopenia, multiple healing fractures
Initial lab evaluation
in suspected Rickets
á CMP, Mg, Phos
á PTH
á 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D
á Long bone x-rays
Vitamin D supplementation for infants: 400 IU Cholecalciferol daily, beginning in first few days of life. Continue until taking 32 oz formula a day or, if breast-fed, until transition to Vit D–fortified cow milk.
Neurology
Epilepsy
CLASSIFICATION OF
SEIZURE
á
Generalized
Seizures: involves entire body without focality. No aura.
o
Tonic/clonic
¤
Whole-body stiffening with LOC followed by
whole-body rhythmic jerks
o
Absence seizures
¤
Brief staring spells, can be 100s per day,
common ages 4-12 yrs
¤
EEG shows 3 Hz spike and wave, provoked by
hyperventilation
o
Atonic seizures (drop seizures)
¤
Generalized loss of tone causing collapse
¤
Most common in ages 2-5 yrs
o
Myoclonic seizures
¤
Sudden, brief contractions of the childÕs entire
body, face, or trunk.
á Partial Seizures: involves one part or side of the body. May generalize after focal onset
o Simple partial seizures: motor, sensory, or autonomic. No change in mental status.
o Complex partial seizures: involve impairment/alteration of consciousness.
¤ May include: automatisms, aura, dŽjˆ vu, or semi-purposeful movements.
á Was the seizure provoked or unprovoked? Triggers include:
o Electrolyte disturbance: low Na, low Ca
o Hypoglycemia
o Hyperammonemia
o Drugs (including illicit drugs – teens!)
o Head trauma
o Meningitis/encephalitis
o Malignant HTN
o Brain mass, hemorrhage, or malformation
SPECIFIC TYPES OF SEIZURE
á
Febrile
Seizures
o
Simple FS:
generalized, less than 15 minutes, no more than 1 per 24 hours, in a
developmentally normal child with T >101, no past hx of seizures, age 6 m
– 6 y
o
Complex FS:
fails to meet all criteria for simple FS
o
Nearly all resolve by 5-6 years
á
Neonatal
Seizures
o
Variable presentation: repetitive contractions,
sustained posturing, ÒbicyclingÓ, tongue thrusting, or eye deviation.
o
Due to the neonateÕs immature neurologic system,
generalized seizures are rare.
á
Infantile
Spasms
o
Most common 3months – 1 year of age
o
Typically presents as clusters of repetitive
truncal flexor/extensor spasms
o
EEG shows hypsarrhythmia
o
Associated with Tuberous Sclerosis
o
Treatment: ACTH
á
Juvenile
Myoclonic Epilepsy
o
Myoclonic jerks in the early morning
o
Absence seizures
o
Generalized tonic/clonic seizures on wakening
o
Usually complete response to AED (valproic acid
is TOC), but need lifelong treatment
á
Benign
Epilepsy with Centritemporal Spikes (Benign Rolandic Epilepsy)
o
Most common seizure type is simple
partial, most during sleep
o
Often comes to medical attention with
secondarily generalized seizure, often during sleep
o
Peak onset in school age; most resolve by
adolescence
o
Treatment often not recommended (other than
abortive therapy rx)
á
Imitators
of seizures
o
Syncope
o
Breath-holding spells
o
Night terrors
o
GERD in infants (Sandifer Syndrome)
o
Benign sleep myoclonus (neonates)
o
Tremors
o
Motor tics
EVALUATION AND MANAGEMENT
á
First-time
afebrile seizure
o History: special attention to birth hx, development, hx of trauma
o Exam: complete neuro exam, head circumference, funduscopic exam, skin exam
¤ If not yet back to baseline, is there concern for subclinical seizures?
o Labs
¤ Not helpful in first generalized seizure with no history of inciting event, brief post-ictal state, and full return to baseline in a developmentally normal child
¤ Consider if H&P findings suggest underlying etiology (a provoked or secondary seizure), if seizure prolonged, or if slow or no return to baseline. Choose labs based on clinical suspicion.
á Toddler or teen: donÕt forget UDS
á Neonates:
o Evaluation for bacterial and HSV meningitis
o Electrolytes, ammonia, newborn screens - this is a presentation of IEM
o EEG
¤ Obtain for all new onset seizure except first simple febrile seizure
¤ About 50% will be normal. Higher yield with prolonged or repeat study.
¤ If hx of staring spells, hyperventilate during EEG to provoke absence sz
o MRI – can usually be done as an outpatient. Obtain if:
¤ Focal seizure or focal finding on EEG
¤ History of trauma (may need CT emergently, but MR still indicated)
¤ Focally abnormal neurologic exam
¤ Developmental delay
¤ Strongly consider if age of onset of seizure <1 year or >15 years
o Treatment
¤ Diastat teaching for all patients (older kids: consider intranasal versed)
¤ Consider anti-epileptic if EEG is abnormal
á
Breakthrough
seizure/Increased seizure activity in patient with known epilepsy
o History: looking for specific trigger
¤ Missed doses of medication, fever, infection, change in diet (ketogenic?), ne w medications or change in dosage, trauma
á Many liquid meds are sugar syrups. Can affect ketogenic diet.
¤ Abortive therapy – was it used? Did it work?
¤ Review outpatient neurology notes for hx and plan for increasing dosage if necessary
o Exam: complete physical and neuro exam
¤ Is the patient back to baseline? If not, is there concern for subclinical status? If so, stat EEG
o Labs
¤ Check therapeutic level of anti-epileptic medication unless dose was changed within last 2-3 days
o EEG
¤ If change in seizure type, to characterize new type of movement or spell
á Febrile Seizure
o Simple febrile seizure
¤ Distat rx and teaching
¤ Consider EEG if first febrile seizure at >3 yr or any febrile seizure > 5 yr
¤ LP if persistent AMS or clinical concern for meningitis
á Strongly consider LP if age <1 yr: meningeal signs are unreliable
¤ Treat underlying cause of fever
o Complex febrile seizure
¤ Diastat Rx and teaching
¤ Routine EEG
¤ If seizure or EEG is focal, MRI
¤ LP if concern for meningitis/encephalitis or encephalopathy
¤ If hx of recurrent prolonged febrile seizure, consider genetic test for Dravet syndrome (SCN1A gene)
á Status epilepticus – requires PICU admission
o Variable definition. Loosely, at least 5-10 min of continuous seizure activity or clustering of seizures that is unresponsive to abortive therapy
¤ Longer time course is acceptable in partial seizure or absence
o Treatment algorithm:
¤ Lorazepam 0.1 mg/kg (max 4 mg), repeat once after 3-5 more minutes if no response. Then, if no response
¤ Fosphenytoin load 20 mgPE/kg. Then, if no response,
¤ Phenobarbital 20 mg/kg
¤ If still refractory, may require intubation and midazolam drip
Stroke
Presentation
á Acute focal neurologic disturbance: most commonly acute hemiparesis
á Less commonly, can be subacute or multifocal/generalized neurologic dysfunction
Pathophysiology
á Most common in children:
o Embolic from thrombus or heart disease
o Ischemic from sickle cell disease
o Unknown etiology – a large percentage
Localization
á
Anterior circulation (carotid, anterior cerebral
or middle cerebral distribution)
- Language
difficulty and right hemiparesis suggest left carotid or left MCA
- Left
hemiparesis suggests right carotid or right MCA
- Posterior
circulation (vertebral and/or basilar distribution)
o
Vertigo, cranial nerve signs/symptoms
Differential
Diagnosis –some of the more common
conditions, but not an exhaustive list!!
- Complicated migraine
- Seizure +/- ToddÕs paralysis
- Hypertensive Encephalopathy/PRES
- MELAS
- ADEM/MS and other demyelinating processes
- Brain Tumor
- Infection: intracranial abscess, encephalitis
- Subdural/Epidural hemorrhage
- Cerebral venous sinus thrombosis
- Alternating hemiplegia of childhood
Etiology
- Sickle Cell disease – the most common predisposing factor
- Heart disease
- Congenital heart disease, esp. post-op from repair or ECMO
- Acquired heart disease: cardiomyopathy, endocarditis, prosthetic valve
- Inherited prothrombotic state – the more common conditions include:
- Protein C or S deficiency
- Factor V Leiden
- Antithrombin III deficiency
- Antiphospholipid syndrome
- MTHFR mutation (elevated homocysteine)
- Other prothrombotic state:
- Combined OCP use
- Smoking
- Pregnancy
- Protein loss (protein-losing enteropathy, nephrotic syndrome)
- DIC
- Malignancy
- Iron-deficiency anemia
- Vascular disease:
- Moya moya
- AVM, cerebral aneurysm
- Fibromuscular dysplasia
- Vasospasm: cocaine use, migraine
- Vasculitis: SLE, Kawasaki, Takayasu arteritis
- Connective tissue disease ˆ arterial dissection (Marfan, Ehlers-Danlos)
- Infection: Varicella (post-infectious), Meningitis, HIV
EVALUATION
- ABCs – pay attention to BP
- MRI/MRA investigation of choice, include imaging of cervical and proximal intracranial arterial vasculature
- ÒBrain attackÓ MRI is faster than standard MRI – discuss with neuro whether appropriate
- CT if MRI not readily available
- Initial labs:
- CBC, BMP, PT/INR, PTT
- Other studies to consider as guided by history and exam:
- ANA, antiphospholipid profile
- Urine drug screen
- Lipid panel
- Prothrombotic w/u in consultation with neuro and heme/onc
- Metabolic work-up in consultation with neuro
ACUTE MANAGEMENT
- ABCs
- BP: do not treat to lower BP acutely until consultation with neuro/neurosurg
- Consult neurology/neurosurgery
- Anticoagulation is decided case by case and may be indicated if:
- Cerebral venous sinus thrombosis
- Cardiac source of embolism
- Arterial dissection
- Known hypercoagulable state
- If sickle cell disease: See Sickle Cell Disease section on CVAs
Ataxia
Definition
á A disruption in smooth coordination of movement most often manifested by unsteady gait and/or tremor
Causes and DDx
á
Life-threatening and urgent:
o
Posterior fossa tumor
o
Ischemic/embolic stroke
o
Hydrocephalus
o
Intracranial hemorrhage
o
Infection: abscess, meningitis/encephalitis
á
Non life-threatening/non-urgent
o
Vestibular dysfunction/labyrinthitis
o
Acute cerebellar ataxia
o
Tick ataxia
o
ADEM
o
Guillan-Barre (acute sensory ataxia)
o
Miller-Fisher syndrome (G-B variant, presents as
cerebellar ataxia)
o
Malformation: Chiari, Dandy-Walker
o
Ingestion: antihistamine, anticonvulsant,
alcohols
o
Trauma/post-concussive syndrome
o Opsoclonus-Myoclonus
o Complicated migraine
o Peripheral neuropathy
o Muscular weakness: myopathy, myositis
á Hereditary disorders:
o FriederichÕs Ataxia (autosomal recessive)
o Ataxia Telangiectasia (autosomal recessive)
o Adrenoleukodystrophies (x-linked)
o Metabolic disorders: Hartnup disease, MSUD, pyruvate dehydrogenase deficiency
o Dominant recurrent ataxias: familial ion-channel disorders
á Also consider, as a diagnosis of exclusion:
o Conversion disorder
o Factitious
Pertinent History
- Onset and duration
- Fever, headache, vomiting, photophobia, vertigo, AMS, diplopia, paraesthesias, weakness, tremor
- Developmental screen
- Recent infection, seizure, head injury, or environmental exposures
- FH of migraine, ataxia, or neurologic disease
Physical Exam -
Localization
á Cerebellar Ataxia
o Wide based gait
o Truncal ataxia (with sitting and standing)
o Head bobbing
o Dysmetria
o Nystagmus
á Sensory Ataxia (involving position and vibration sense)
o High stepping gait/ slapping feet down
o Abnormal proprioception (toes)
o Diminished reflexes
o Abnormal Romberg test
WORKUP
Guided by history and exam.
á Imaging:
o CT only if emergent, concern for herniation or mass effect before doing LP
¤ Poor visualization of posterior fossa (cerebellum!)
o MRI indicated if need to evaluate posterior fossa, dem
o Consider MRI of spinal cord based on exam
á Labs to consider
o UDS
o Metabolic labs: CMP, ammonia, serum/urine amino acids, urine organic acids, lactate, pyruvate
o CPK
o LP: elevated protein in ADEM, MS, Guillian-Barre/Miller-Fisher
¤ Oligoclonal bands for MS
¤ CSF lactate/pyruvate for metabolic concerns
¤ Image first if concern for elevated ICP
o Concern for neuroblastoma: CXR, abdominal US, urine HVA/VMA
á EEG: in patients with altered consciousness, fluctuating clinical signs
Headache
This
section includes more common diagnoses but is not an exhaustive list.
Primary Headache – should have a normal neurologic exam.
á Migraine: classically dull pain progressing to throbbing/pulsating pain, unilateral or bilateral, most often over the temples and around/behind the eyes. Often w/ photophobia, phonophobia, nausea, malaise, fatigue
o Migraine without aura: no preceding sensory disturbance
¤ Menstrual migraine usually does not have aura
o Migraine with aura: preceded by visual disturbance or dysesthesia
¤ Typical aura: visual, sensory, or verbal symptoms but no motor weakness
¤ Hemiplegic migraine: transient hemiplegia associated
¤ Migraine with brainstem aura: complex migraine that may also include vertigo/ataxia and occipital rather than frontal/temporal pain
¤ Retinal migraine: rare. Abrupt visual loss or disturbance in one eye followed by ipsilateral periorbital pain
o Status migrainosus: migraine lasting >24 hrs
o Cyclical vomiting – a migraine variant
á
Tension
o Global headache, neck tenderness and muscle spasm. Often a pressure-like sensation
o Can be episodic, chronic, or associated with life stressors
á
Cluster
headache (Trigeminal autonomic cephalalgia)
o
Unilateral, around eye or temple
o
Rapid onset, excruciating pain, 30 min-3 hrs
o
May have ipsilateral lacrimation, rhinorrhea,
sweating, Horner syndrome
Secondary Headache
á Acute febrile illness: viral illness by far the most common. Also strep.
á Concussion/post-traumatic: remember to consider epidural/subdural hematoma
o Concussive HA should have normal exam
á Analgesic rebound from overuse of meds, esp NSAIDs
á Hypertension –acute rise, often secondary HTN
á Infection: sinusitis, intracranial abscess, meningitis, encephalitis
á Idiopathic intracranial hypertension (pseudotumor cerebri)
á Intracranial hemorrhage – sudden, severe
á Brain tumor
o Warming signs include: AM headaches or headache wakes from sleep, AM vomiting, progressive over time, focal neurologic signs associated, age <3 years (when benign headaches less common)
Evaluation
á Complete history with close attention to:
o Onset – acute v chronic
o Family hx of headache, motion sickness
o Location, quality, frequency of pain
o Precipitating, aggravating/alleviating factors
o All current medications, Analgesics used, frequency, dose
o Conditions listed under Òsecondary headacheÓ above
á Complete exam with close attention to:
o Vitals, especially BP
o Eye exam including funduscopic exam, visual fields
o Complete neurologic exam
á Indications for imaging (non-contrast MRI unless emergent)
o Abnormal neurologic exam
o Early AM headaches and/or waking from sleep with headache
o Signs of increased ICP (must image before LP) **if concern for mass, use contrast MRI
o Concern for intracranial infection (meningitis, epidural abscess, LemierreÕs)
o Rapidly increasing headache frequency or sudden onset of headaches
Management of Status Migrainosus Inpatient/ED
á Eliminate all screens: TV, phone, tablet, computer
á First-line abortive therapy:
o Toradol 0.5 mg/kg to max of 30 mg q6 hrs if no contraindication
¤ Use Zantac or PPI for gastric protection
o If contra-indicated, use either:
¤ Metoclopramide (Reglan) 0.1-0.2 mg/kg/dose, max 10 mg OR:
¤ Prochlorperazine (Compazine) 0.1-0.15 mg/kg/dose, max 10 mg
á
If the above fails: Dihydroergotamine (DHE)
protocol. DHE may cause
nausea/vomiting, high BP, vasospasm ˆ
TIA, stroke, MI.
o Contra-indications to DHE include:
¤ Hemiplegic or basilar migraine
¤ Use of triptan within 24 hours
¤ Uncontrolled HTN
¤ Current use of –azole antifungals, protease inhibitors, macrolides
¤ Hx ischemic heart disease, angina, coronary vasospasm
DHE Protocol
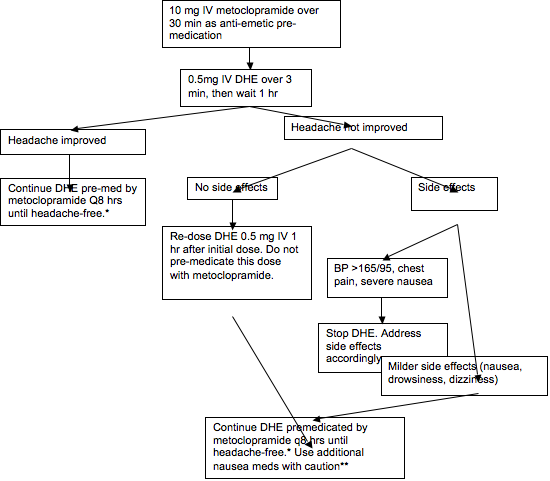
*Should see improvement in headache by dose 5. If continued improvement, can give up to 20 doses.
**Both zofran and phenergan are serotonin modulators and, when used with DHE, there is a risk of serotonin syndrome. If significant nausea persists, could use low-dose (0.05 mg/kg) ativan.
Migraine Prophylaxis
– consider when >2 migraines per week or disabling. Start at the lowest dose and titrate slowly
every 2-3 weeks. Adequate trial of medication depends on frequency of headaches
and could be 2-3 months.
á Cyproheptadine: 2-4 mg PO QHS, BID, or TID. Max 16 mg/day
o More effective for younger children (7-9 years)
o Can be sedating, cause increased appetite leading to weight gain
á Amitriptyline/Notriptyline: 5-40 mg PO QHS. Start at lowest dose, titrate Q2-3 weeks to effect
o Significant overdose can cause fatal arrhythmia (widened QRS ˆ v-tach)
á Topiramate: 1-3 (max 5) mg/kg/day divided BID. Absolute max 50 mg BID.
o Alternative to cyproheptadine in younger children
o Can decrease appetite resulting in weight loss
o Can affect short-term memory
á Depakote (age 16+): 250 mg PO BID, can increase to max fo 1000 mg BID.
á Depakote ER (age 16+): 500 mg PO daily, can increase to 1000 mg after 1 week
á Propranolol: 0.6-1.5 mg/kg/day divided Q8hrs. Max dose 4 mg/kg/day or 120 mg/day
o Alternative dosing: </= 35 kg: 10-20 mg TID. >35 kg 20-40 mg TID
o Can cause fatigue, decreased energy
o Avoid in patients with asthma
Cardiology
Chest Pain
95-99% of non-traumatic chest pain in children is not the result of a
severe condition. There is a vast differential diagnosis. This is not an exhaustive
list of conditions causing chest pain but includes the more common benign and
severe conditions to assist in forming your differential diagnosis and starting
your evaluation.
Common
Conditions
á
Musculoskeletal
o
Muscle strain
o
Costochondritis
o
Tietze syndrome
o
Precordial catch
o
Pectus
excavatum/carinatum
á
Psychiatric
o
Anxiety
o
Panic attack
o
Depression
o
Somatization
á
Respiratory
o
Asthma
o
Pneumonia
o
Chronic cough
leading to MSK pain, even fracture
o
Cough leading to
pneumomediastinum
á
Gastrointestinal
o
GERD
o
Esophagitis
o
Esophageal foreign
body
o
Esophageal
spasm/dysmotility, achalasia
o
Gastritis/peptic
ulcer
o
Cholecystitis
o
Pancreatitis
á
Breast
o
Males: gynecomastia.
Rare.
o
Females: cyclic pain
with menses, fibrocystic change, thelarche, pregnancy
á
Other
o
Shingles
o
Pleurodynia
History most compatible with benign chest pain
á
Sharp, brief,
non-radiating, non-exertional chest pain exacerbated by palpation, chest wall
movement and/or deep inspiration.
Potentially
Life-threatening conditions and associated classic (but not universal) presentations
á
Cardiac
o
Myocardial
infarction
¤
Crushing, substernal
pain /pressure, radiation to L arm or jaw, associated vomiting, sweating
– most often occurring during exercise
o
Variant angina
(drugs – cocaine, bath salts, synthetic variants or decongestants)
¤
Anginal pain as
above, hx of drug use
o
Hypertrophic
cardiomyopathy
¤
Chest pain and/or
¤
Exertional syncope
or dizziness
o
Tachyarrhythmia
¤
Palpitations (may be
perceived as chest pain/discomfort), syncope without prodrome esp. with
exertion
o
Aortic
dissection/aneurysm
¤
Tearing chest pain
radiating to back
o
Anomalous coronary
artery
¤
Classic angina with
exertion
¤
Exertional syncope
or dizziness
o
Myocarditis
¤
Nonexertional and/or
exertional, often constant, chest pain or exercise intolerance, shortness of
breath, easy fatigue, tachypnea
o
Pericarditis
¤
Substernal pain
(sometimes radiating to the back), worse when supine, improved by leaning
forward
á
Pulmonary
o
Airway foreign body
¤
Respiratory
distress, drooling, monophonic wheezes throughout
o
Pneumothorax
¤
Asymmetric breath
sounds and chest movement, +/- tracheal deviation, respiratory distress
o
Pulmonary embolism
¤
Tachycardia,
dyspnea, hypoxia
o
Acute chest syndrome
á
Other
o
Spinal cord
compression
¤
Focal neurologic
signs associated with location of lesion
o
Mediastinal mass
¤ Substernal pain, dyspnea, orthopnea
á
Findings concerning
for a severe underlying condition in general:
o
History
¤
Exertional syncope
¤
Classic angina:
crushing substernal pain +/- radiation to L arm, jaw, nausea, vomiting,
sweating
¤
Retrosternal pain
radiating to the back or shoulder
¤
Orthopnea or
worsening of pain when supine
¤
Exercise intolerance
due to shortness of breath
¤
In infants,
sweating, difficulty with feeds, paroxysmal agitation
o
Exam
¤
Fever associated
with acute onset of pain
¤
Abnormal BP for age,
high or low
¤
Narrow pulse
pressure with tachycardia
¤
Tachypnea or
tachycardia for age
¤
Gallop rhythm
¤
Murmur
¤
Significantly
abnormal lung exam: lack of breath sounds on one side, asymmetric chest wall
movement, respiratory distress
Further Evaluation
á Benign cause diagnosed by history and physical exam
o No further testing indicated
o Symptomatic treatment as needed (i.e. for GERD, costochondritis), follow-up
á When should an EKG and/or Echo be considered?
o Concern for cardiac cause of chest pain
o Inability to definitively diagnose non-cardiac cause
o Exertional chest pain
o Chest pain with fever
o Chest pain radiating to the back or jaw or that is worse when supine
o Hx of congenital heart disease, Kawasaki, collagen vascular disease, hypercoagulable state (thrombophilia, immobility)
o Exam findings concerning for pathologic murmur, heart failure, pericardial effusion, or tamponade
o Abnormal EKG
á Other studies pertinent to the individual patient
Congestive Heart Failure
ETIOLOGY
CHF may result from congenital or acquired heart diseases with volume and/or pressure overload or from myocardial dysfunction.
- Congenital Heart Disease: most common cause in pediatric age group
- Pulmonary overcirculation due to left to right shunting; pressure overload
- Uncommon: anomalous left coronary artery from the pulmonary artery leading to myocardial infarction.
- Acquired Heart Disease: Rheumatic Fever, Collage Vascular Disorders, Vitamin deficiencies, Kawasaki Disease
- Myocardial Dysfunction: Myocarditis, Endocardial fibroelastosis, Metabolic abnormalities, Adverse Effects of Medications, Various muscular dystrophies (classically Duchenne/BeckerÕs)
- Arrhythmia: Tachyarrhythmias (SVT), Bradyarrhythmias (AV Block)
- Miscellaneous: Acute Hypertension (including upper extremity hypertension in neonate with critical coarctation), Severe anemia, Volume overload, Sepsis
CLINICAL
MANIFESTATIONS
History
- Neonates/infants:
- Tachypnea and grunting
- Fussy
- Poor feeding (sweating, increased RR, tiring with feeds)
- Poor weight gain; Linear velocity usually maintained
- Children
- Easy fatigability
- Shortness of breath
- Orthopnea
- Swelling (less common in younger children; rare if CHF caused by pulmonary overcirculation)
Physical Exam
á General:
- Tachycardia and tachypnea
- Gallop rhythm
- Heart murmur (could be systolic and/or diastolic)
- Cyanosis (more often peripheral than central)
- Weak pulses (assess for upper/lower extremity asymmetry)
- Hepatomegaly; Splenomegaly; Overactive precordium
- Peripheral edema is rarely seen in
infants with CHF
á Left-sided Failure
- Tachypnea
- Orthopnea
- Wheezing and pulmonary crackles
- Decreased and/or asymmetric breath sounds with pleural effusion(s)
á Right-sided Failure
- Hepatosplenomegaly
- Physical findings consistent with pleural effusion, ascites
- Edema: eyelid/facial, sacral, lower extremity (less frequent)
Studies
á Chest x-ray
- Cardiomegaly and increased vascular markings, pleural effusion
á ECG
- May show signs of LVH and/or RVH
- Left axis deviation in AV septal defects, Tricuspid atresia
á Echocardiography
- Diagnostic for a congenital or acquired heart defect
- Evaluates systolic and diastolic cardiac function
MANAGEMENT
Acute CHF
- Elevate head of bed (in the older patient)
- Oxygen unless CHF suspected to be due to congenital heart disease with pulmonary overcirculation
- Treat volume overload (Diuretics)
- Inotropic support if unstable:
- Milrinone: inotrope and vasodilator
- Dobutamine: inotrope and vasodilator
- Dopamine: combination of alpha-1, beta-1, dopamine agonist depending on dose
- PGE-1 for ductal-dependent congenital heart lesions
- Treat underlying causes (hypertension, arrhythmias, pericardial effusion)
- Correct electrolyte imbalances
Chronic CHF
á Diuretics: reduce preload. May eliminate need for inotrope (digoxin)
o Lasix 1-4 mg/kg/day, po in 1 to 4 divided doses
¤ Starting dose 1 mg/kg/dose. Can use up to 4x/day
¤ Side effects: hypo-K, hypo-Cl, hypo-Na, alkalosis, dehydration
á Electrolyte abnormalities predispose to digoxin toxicity!
o Spironolactone 1-3mg/kg/day po in 2-4 divided doses
¤ Use with Lasix to increase diuresis without losing too much K
¤ Consider adding when Lasix needs >2 mg/kg/day
á Digoxin
o Increases calcium influx into myocardial cell ˆ increased contractility
o Do not use if: HOCM, complete heart block, WPW, cardiac tamponade, myocarditis
o Common ECG effects:
¤ shortening of QTc (earliest sign); sagging ST segment; diminished amplitude, inverted, biphasic T-waves; slowing of heart rate
o Digitalis Toxicity
¤ Non-cardiac symptoms: nausea, vomiting, diarrhea, restlessness, drowsiness, fatigue and visual disturbances in older children
¤ ECG signs: prolonged PR interval, bradycardia or SA block, prominent U waves, J-point depression, arrhythmias.
¤ Factors that exacerbate toxicity: hypo-K, hypo-Mg, low T4, and hyper-Ca
á ACE-inhibitors (Enalapril, Captopril)
o Reduce systemic afterload
o Adverse reactions:
¤ neutropenia, angioedema, cough, azotemia, hyperkalemia, rash
o Caution with ACE-I and K-sparing diuretic ˆ hyperkalemia
Hematology/Oncology
Fever in Immunocompromised Children
The following are guidelines for
patients with fever(T > 101 or >100.5 x2 in 30
min) and neutropenia. This is most specifically pertinent to chemotherapy patients,
but should be considered in any neutropenic patient.
Why so vulnerable?
á Neutropenia ˆ unable to mount a response to bacterial infections
á Chemotherapy also affects immunoglobulin production, cell-mediated immunity
á Chemo interrupts skin and mucous membrane integrity ˆ increased susceptibility
History
á
History of present illness and comprehensive ROS
to help define the source of infection
- Underlying disease
- Recent therapy (e.g., radiation or chemotherapy—meds and dates received)
- Recent surgical procedures, especially central line placement
- Exposures, especially to varicella
- Presence of an indwelling catheter; previous infection of catheter
Physical Exam
** in
the neutropenic patient that the signs of inflammation may be muted or absent.
Pus is created by neutrophils, so you are unlikely to find any even if there is
severe infection
- Thorough sinopulmonary exam to include ears, sinuses, teeth, throat, and lungs
- GI tract with particular attention to the RLQ (typhlitis) and the perianal area (NO RECTAL TEMPS OR SUPPOSITORIES)
- Hepatomegaly and splenomegaly as evidence of fungal or viral infections
- Skin looking for cellulitis, abscess, septic emboli (small erythematous or hemorrhagic papules) or varicella-zoster and examination of indwelling catheter site
- Pain alone may be a sign/location of an
infection
Labs and Studies
- CBC with differential
- Blood culture from all central lines.
- UA and culture in young child or as indicated by H&P – clean catch only. Do not cath.
- PA and lateral CXR in any patient with respiratory symptoms or young age.
- Consider sinus CT, chest CT, abdominal CT as indicated by H&P
- Consider viral titers/PCR for CMV, EBV
- Nasopharyngeal swab for RSV, adenovirus, influenza if indicated
Treatment
- ABCs first
- Goal is abx within 1 hr of presentation. Do not wait for lab results (ANC) to give abx.
- Empiric therapy (i.e., no source is evident) must include Gram negative coverage
- Cefepime
- Ceftriaxone if ANC known to be >500
- Add vancomycin for gram (+) for:
- Mucositis
- Previous line infection
- Toxic appearance
- AML
- Recent procedures
- Add anaerobic coverage if: sinusitis, intra-abdominal infection. Options include:
- Meropenem for Gram (+), gram (-), and anaerobe as single agent
- Clindamycin if anaerobes above the diaphragm
- Metronidazole if intra-abdominal
- Add Voriconazole as fungal coverage for:
- Recent broad-spectrum abx course
- Recent steroid course
- Prologned neutropenia not responding to antibiotics
- Add TMP-SMX to cover pneumocystis jirovecii if interstitial pneumonitis on CXR
- Continue prophylactic TMP-SMX or pentamidine to prevent PCP pneumonia.
Oncologic Emergencies
HYPERLEUKOCYTOSIS (admit
to PICU)
á
Who is at risk
o Newly diagnosed acute leukemia patient with extremely
elevated WBC
¤ In AML, WBC >100K
¤ In ALL, WBC >500K
o NOT at risk: CML, reactive leukocytosis from mature
cells rather than blasts
á
What happens
o Viscosity of blood increases leading to sludging and stasis
in small vessels
o Causes ICH, pulmonary hemorrhage or infarction
á
Evaluation (same as for any newly diagnosed leukemia patient)
o CBC
o Type and screen or cross-match if indicated (see below)
o Tumor lysis labs (BMP, Ca, Phos, Uric Acid, UA)
á
Treatment
o Immediate leukoreduction:
¤ Arrange an emergency leukophoresis to be done by the
American Red Cross (251-6000).
¤ Will need
double lumen renal dialysis catheter placed by surgeons or PICU attending in
femoral vein.
o Maintain plts > 75,000 to avoid CNS bleed
o Do not transfuse RBCs unless Hgb <7 gm/dL to prevent
further increase in viscosity. If Hgb < 7.0, transfuse slowly in 5
cc/kg aliquots.
o Hydrate at 1.5x maintenance provided patient does not
have signs or symptoms of elevated intracranial pressure.
o Alkalinize fluids with 30-50 mEq/L sodium bicarb
o Adjunctive treatment: start induction chemotherapy
¤ Must watch VERY closely for tumor lysis when there is a
large burden of malignant cells
SUPERIOR VENA CAVA SYNDROME (admit to PICU)
á
A mediastinal mass
compressing/occluding the SVC and/or trachea.
o Most common with HodgkinÕs Lymphoma
á
Symptoms:
o stridor, dyspnea
o plethora or cyanosis of the face/neck
o headaches, altered sensorium
o papilledema
á
Management
o Keep patient upright. Do NOT paralyze/sedate for
imaging/procedures
o Secure the airway if any concern for tracheal compression
o Get a diagnosis ASAP to start definitive treatment and
stop/reverse tumor growth
TUMOR
LYSIS SYNDROME
á
Who is at risk:
o Patients with rapidly dividing cells who present with large
tumor burdens (high WBC, massive organomegaly, large mediastinal or other tumor
mass).
á
Manifestations:
o hyperuricemia, hyperkalemia, hyperphosphatemia with associated
hypocalcemia.
o In AML, especially APML, DIC is common.
á Evaluation
o
STAT BMP, Ca, Phos,
Uric acid, UA
o
If elevated
creatinine, US abdomen to r/o ureteral obstruction from mass
¤ Can also show leukemic infiltration of kidneys
o
Frequency of
monitoring labs depends on degree of abnormality and clinical status of patient
á Treatment
o
Aggressive hydration: 2400-4000 cc/m2/day (or 1.5 - 2x
maintenance)
¤ Alkalinization: Using Na-bicarb in
fluids to goal of urine pH 7-8 may
help excretion of uric acid.
¤ If Hb significantly low, may need
PRBC first to avoid CHF
o
To reduce uric acid:
¤ Allopurinol 10 mg/kg/day divided
Q8
á Inhibits xanthine oxidase ˆstops production of uric acid
¤ If severe, Rasburicase 0.15 mg/kg once
á Converts uric acid to allantoin
á DO NOT alkalinize fluids when
using rasburicase
á Rasburicase is contraindicated in patients with G6PD deficiency. Ask
pertinent history, and if concerning, check for G6PD first.
o
Hyperkalemia:
¤ See fluids/electrolytes section
¤ Lasix and alkalinized fluids are
commonly used
o
Hyperphosphatemia:
¤ Amphogel (aluminum hydroxyide) or
calcium carbonate as phosphate binders
Sickle Cell Disease
VASO-OCCLUSIVE
CRISIS: sickled cells occlude microvasculature causing ischemia and
pain that can be severe
á Manifestations
- Children <5 years: often have dactylitis, painful swelling of the hands and feet.
- Older children: Pain can be anywhere. Common sites: abdomen, back, long bones, esp legs
- Mild fever may be associated with VOC. Fever >/= 101 still requires full evaluation (see section on fever in sickle cell disease)
- **Patients with sickle cell disease can have pain that is not due to VOC (e.g., pneumonia, osteomyelitis, pancreatitis, appendicitis, trauma, etc.)
- Evaluation
- Full history and physical to determine trigger for VOC. Pay attention to O2 sat
- CBC with manual diff, retic, BMP if giving ketorolac, consider type & screen based on clinical suspicion of need for PRBC
- CXR if thoracic or back pain with hypoxia, tachypnea, or abnormal lung exam
- If fever, blood culture (see section on fever)
- Other labs as indicated by presentation
- ED management of VOC –Remember that patients may not be opiate-naive!
- Initial evaluation:
- Obtain CBC, BMP, retic
- IF chest pain, hypoxia, or rales: CXR
- IF recent trauma pertinent to pain, consider x-rays
- Initial pain management:
- Initial pain and sedation assessment
- Morphine or hydromorphone, weight-based
- Ketorolac, weight-based
- 1.5x MIVF (unless concern for ACS, then cautious fluids!)
- 10 cc/kg bolus only if clinical dehydration
- Then:
- Repeat opioid at 50% initial dose Q30 min x2 with pain and sedation assessment prior to administration
- AT 3rd dose, give PO opioid in addition to or instead of IV dose based on pain and sedation level
- PO options include: oxycodone +/- tylenol, hydrocodone + Tylenol, Tylenol with codeine
- Disposition:
- d/c home if:
- pain improved from initial score
- pain adequately controlled on oral medication
- patient and parent agree that relief is adequate
- Inpatient management of VOC
- IVF with goal of total intake at 1-1.5x maintenance needs
- Ketorolac 0.5 mg/kg (max 15 mg if < 50 kg, 30 mg if > 50 kg) IV q6 hrs, max 5 days
- Consider H2 blocker or PPI to prevent gastritis
- Morphine 0.1 mg/kg (max 10 mg) IV Q3-4 hrs; hydromorphone instead of morphine it pt prefers
- Rescue dose: 50% of initial opioid dose q2 hrs PRN
- If no relief or pt preference, start morphine PCA (see table below)
- Prophylaxis/Other:
- Albuterol with PEP Q4hrs, incentive spirometry q 1-2 h to prevent ACS; continuous pulse ox (goal >/= 94%)
- Stool softener to prevent constipation
- Ondansetron prn n/v
- Low dose diphenhydramine PRN pruritis
|
Morphine PCA |
|
|
Starting Dose |
Adjustments |
|
|
SICKLE CELL DISEASE AND FEVER (TEMP ³/= 101¡ F): children with sickle cell are at high risk for invasive infection by encapsulated bacteria such as S. pneumo and H. influenza due to functional asplenia
á Evaluation
o Prompt history and physical to evaluate for source of fever
¤ Remember bone/joint pain/tenderness (risk for osteomyelitis)
o CBC-d, retic, blood culture
o If cough, back or chest pain, or hypoxia, CXR
o Other studies as indicated by H&P
á Management
o ABCs first
o IV antibiotics: ceftriaxone 75 mg/kg is treatment of choice
¤ If cephalosporin allergy, ampicillin/sulbactam 50 mg/kg/dose
¤ If penicillin and cephalosporin allergy, meropenem 20 mg/kg/dose
¤ If unstable or concern for CNS infection, add vancomycin 10-15 mg/kg
o
Admission
criteria – any one of the following:
¤ Temp ³ 103.1
¤ Ill-appearance
¤ WBC > 30K or < 5K μL
¤ Plt < 100K μL
¤ Hgb < 5g/dL
¤ History of sepsis
¤ Infiltrate on CXR or abnormal O2 saturation
¤ Cephalosporin allergy – due to need for frequent abx dosing
¤ Unable to ensure follow-up
o
Can
discharge if all of the following criteria are met:
¤ Clinically stable 3 hrs after ceftriaxone
¤ Compliant with PCN ppx, Immunizations UTD
¤ Stable social situation and able to follow up the next day (min phone call)
¤ Rx 7 day course of cefdinir (cover while blood culture pending)
o Inpatient, continue abx until afebrile and blood cx NG x 24 hrs
ACUTE CHEST SYNDROME: defined as a new infiltrate on chest x-ray with pulmonary symptoms (chest pain, cough, hypoxia, tachypnea, retractions, etc.) and/or fever.
á Etiology multifactorial:
o Atypical bacteria such as mycoplasma or chlamydia– most common identifiable infectious etiology
o Bacterial pneumonia, viral infection
o Fat embolism
o Pulmonary infarction from sickling
o Increase risk of ACS if:
¤ VOC w/ pain leading to shallow breathing, atelectasis
¤ Respiratory depression from opioids
¤ Over-hydration
¤ Asthma, chronic hypoxia
á Evaluation
o ABCs!
o CBC-d, retic, type and cross-match leukodepleted, antigen matched, sickle negative PRBCs
o CXR
á Management
o Give O2 to maintain sat >/= 94%
o Analgesia (see above)
¤
Over-medication can cause respiratory depression
but under-treating leads to splinting that worsens ACS. Must adequately treat pain!
¤
Continuous pulse-ox, ETCO2 monitor if on PCA or
high opioids doses
o Hydration – total intake no more than 1x maintenance
o Antibiotics: Ceftriaxone + azithromycin
¤ Add clindamycin if concerned about MRSA
¤ Add vancomycin if critically ill
o Albuterol + PEP Q4hrs
o Incentive spirometry Q1-2 hrs while awake (pinwheel in young children)
o Consider need for CPAP or BiPAP – would mean PICU admission
o If no improvement in 12-24 hrs or symptomatic anemia, transfuse 10 cc/kg PRBC; avoid hypertransfusion/hyperviscosity (keep hgb < 12)
¤ If Hgb >10 or critically ill, may need exchange transfusion
ACUTE SPLENIC SEQUESTRATION: sudden trapping of RBCs in spleen causing drop in Hgb >/= 2 gm below baseline and increase in spleen >/= 2 cm than baseline.
á Manifestations
o Abdominal pain, rapidly enlarging spleen
o Tachycardia, hypotension if severe
o Occurs before auto-infarct spleen
¤ <5 years most common in HbSS
¤ Any age in HbSC or HbS Beta + Thalassemia
á Evaluation
o ABCs first: if hypotensive, stabilize with saline boluses while awaiting PRBC
o CBC (usually plts low), retic (usually high, but may be low if associated with aplastic crisis),
o BMP or CMP,
o Type and cross-match leukodepleted, antigen matched, sickle negative PRBCs
á Treatment
o Transfuse 5 cc/kg PRBC aliquots to goal hgb 8-9 (ask blood bank to split unit into 2-4 aliquots to avoid exposure to multiple donors); expect ÒautotransfusionÓ as spleen releases sequestered blood cells
o If donÕt have time to get antigen matched PRBCs, give C, E, Kell negative PRBCs; if emergent, use emergency-release O-negative blood
o 50% risk of recurrence after one episode and significant mortality associated. Splenectomy recommended after first severe acute episode.
CEREBROVASCULAR ACCIDENTS: most are thrombotic/ischemic, but young adults can have hemorrhagic strokes as well
á Manifestations
o Acute hemiparesis, Slurred speech, or facial droop
o Seizure
o Altered mental status
á Evaluation
o CBC, retic, type and cross match PRBCs for exchange transfusion (C, E, Kell negative, sickle negative, leukodepleted)
o CMP
o hemoglobin electrophoresis
o MRI/MRA without contrast as quickly as possible
o If MR unavailable, need CT without contrast to r/o hemorrhage
á Treatment for infarctive stroke
o Exchange transfusion by American Red Cross pheresis team (803-251-6074) with goal to reduce % sickled cells to 30% and get hematocrit 30%
o Need double lumen femoral line by PICU
PRIAPISM: painful erection due to sickling and venous occlusion in the corpora cavernosa. High risk of impotence in patients with untreated priapism.
á Management
o First: hydration, analgesia, heat, pseudoephedrine or terbutaline, frequent voiding
o If lasts 4 hours, aspiration and irrigation with phenylephrine
o May need Winter shunt if persistent despite aspiration/irrigation
o If severe or recurrent, consider prophylaxis – at discretion of heme-onc
APLASTIC CRISIS: Decrease in Hgb (1 gm/day) and in retic count due to arrest of erythropoiesis from viral infection.
á Manifestations:
o Fatigue, pallor
o CHF, edema, tachycardia
á Evaluation:
o CBC-d, retic, type and cross-match leukodepleted, antigen matched, sickle negative PRBCs
o Consider Parvovirus IgG and IgM or other viral studies as indicated
á Treatment:
o Transfuse if symptomatic from anemia and/or if Hgb <5 without increasing retic. Transfuse 5-10 cc/kg (ask blood bank to split unit into 2-4 aliquots to avoid exposure to multiple donors), slowly!
o Avoid hypertransfusion/hyperviscosity (keep hgb < 12).
o
Furosemide 1 mg/kg to max 40 mg if fluid
overload
Anemia
Classification
– this is not an exhaustive list,
but a list of more common diagnoses to consider
á First stratifier:
o Isolated anemia: other cell lines normal
o Other cell lines abnormal:
¤ Anemia and low plts: HUS, TTP, DIC, Evans Syndrome
¤ Anemia and high plts: Fe deficiency, infection, post-splenectomy
¤ Pancytopenia: aplastic anemia, leukemia, myelodysplasia, drugs/toxins, B12/folate deficiency, hypersplenism
¤ Anemia and leukocytosis: infection, leukemia
á Isolated Anemia, by etiology:
o Decreased production (low retic)
o Increased destruction (high retic)
o Blood loss
á Isolated Anemia, By RBC size
o Microcytic
¤ Iron deficiency
¤ Thalassemia
¤ Anemia of chronic disease
¤ Consider lead poisoning concurrent with iron deficiency in at risk patients
o Normocytic
¤ Hemolytic anemias (high retic)
á Autoimmune
á MAHA (TTP, HUS, DIC, Kasabach-Merritt)
á Enzyme defect
á Membrane defect
á Hemoglobinopathy
¤ Normal or low retic
á Blood loss
á Aplastic conditions – TEC
á Infection
á Anemia of chronic disease
á Renal disease
á Lead poisoning
o Macrocytic
¤ Bone marrow failure
á Myelodysplastic syndromes
á Diamond-Blackfan anemia
¤ B12 or Folate deficiency
á Folate deficiency can complicate sickle cell disease
á Methotrexate ˆ folate deficiency
¤ Down Syndrome
¤ Liver disease
¤ Hypothyroidism
¤ Post-splenectomy
¤ Reticulocytosis (normal mature RBCs but many reticulocytes makes average size (MCV) elevated)
Evaluation of child with isolated anemia
á CBC with manual differential, retic
o Low MCV: most common causes are iron deficiency and thalassemia ( alpha or Beta thal) minor. Pay attention to ethnicity (Asian, African-American, Mediterranean more likely to have thalassemia)
¤ Diet history.
á If low iron, lots of milk, in a young child: trial of iron therapy
o RDW high in iron deficiency
á If diet is sufficient, check TIBC, Fe, ferritin, transferrin levels, consider checking stools for heme
á Consider inflammatory bowel disease in patients with iron deficiency anemia if appropriate age/history
¤ If normal Fe studies, Hgb electrophoresis
á Electrophoresis will NOT definitively diagnose thalassemias
á Most β-thal patients will have high HbA2 but lack of this does not exclude it
á Most β-thal patients will have normal to high serum iron, ferritin, low MCV, high RDW, and increased RBC count
o Normal MCV:
¤ High retic: hemolysis or hemorrhage. Look at smear for evidence of hemolysis and specific etiology:
á Schistocytes, spherocytes/elliptocytes, sickle cells
¤ Low retic: see ddx above. If underlying etiology not clear, may need bone marrow biopsy
o High MCV:
¤ Specific testing as indicated by peripheral smear. Examples:
á Hypersegmented PMNs ˆ B12/folate deficiency
á Consider bone marrow for myelodysplastic syndrome
Transfusions
RED BLOOD CELLS
á
Format
o
PRBC = packed red blood cells. Hct of 66%
o
One unit is approx 250 mL (remember that unit
size varies)
o
Transfuse over 3-4hr depending on clinical
status of patient
¤
Risk of fluid overload = transfuse more slowly
á
Calculations
o
Commonly used: 15 cc/kg PRBC should raise Hgb by
3 g/dL
- Vol cells (mL)= Est.
blood volume x desired change in hct
Hct of pRBC
á Wait 4 hrs after transfusion to repeat H/H if repeat testing is needed
PLATELETS
á
Format
o A platelet pheresis is a single donor product. Vol about 250-300 mL.
o Transfuse over 1 hr OR no more than 10 cc/kg/hr
á Calculations
o Children <15 kg: 10-15 mL/kg will raise platelet count by 50-100,000
o Children >15 kg: 1 pheresis pack
á Wait one hour to check platelet count if necessary to repeat
SPECIAL CONSIDERATIONS
- All PRBCs are now leukodepleted
- Irradiated products: protect against Graft v. Host Disease (GVHD)
- Use for all oncology patients, NICU/newborn patients
- Cytomegalovirus: extremely common in the population. Can be severe in newborns and oncology patients. Leukodepletion removes CMV
- CMV negative products are not necessary in routine oncology patients
- follow NICU guidelines for NICU patients
- Sickle cell disease: blood must be:
- Sickle-dex negative (excludes donors with sickle cell trait)
- Antigen matched (to minimize development of antibodies against donor blood)
- If patient has not received PRBCs previously, send blood for RBC phenotype.
- Type
and Screen
- Order placed when a patient MAY need a transfusion
- Type
and Crossmatch
- Order placed when immediate transfusion is necessary; volume must be ordered
- Transfusion reaction: new fever/hives/wheezing
- Stop transfusion
- Treat with ABCÕs, Tylenol/benedryl. May need steroids if severe or refractory
- Premedications/Indications
- Prior febrile or allergic reaction to that blood product
- Tylenol and benadryl
Venous Thrombosis and Thromboembolism
|
Risk Factors for Thrombosis |
|
|
Acquired |
Inherited |
|
Central Venous Line# Congenital Heart Disease Trauma TPN Infection Surgery and Immobilization Oral Contraceptive Use Obesity Nephrotic Syndrome Inflammatory Bowel Disease Diabetes Mellitus Systemic Lupus Erythematosus Antiphospholipid Syndrome (Lupus Anticoagulant, Anticardiolipin Ab)* |
Antithrombin III Deficiency* Protein C Deficiency* Protein S Deficiency* Factor V Leiden Mutation* Prothrombin Gene Defect* Increased Factor VIII Increased Fibrinogen, Dysfibrinogenemia Plasminogen Deficiency Homocysteinuria*(fasting) Lab evaluation should be considered in certain but not all situations. See below. *Labs most commonly drawn if applicable |
# 2/3 of DVTs in children are associated with CVLs!
á Presentation:
o DVT: Swelling, pain, discoloration of affected limb
o PE: dyspnea, tachypnea, hypoxia, hemoptysis, pleuritic chest pain
¤ Fever in up to 20%
o Central line-associated: line will not draw back or infuse
á Evaluation
o **D-dimer:
¤ Elevated D-dimer is sensitive but has VERY poor specificity.
¤ Normal D-dimer has good negative predictive value.
o Hyper coagulation evaluation:
¤ NOT usually indicated in cases that are truly provoked
á dehydration, CVL, infection, OCPs, surgery/immobilization
¤ Consider in:
á Infants, especially with massive, multiple, or cutaneous signs (purpura fulimans)
o Anti-thrombin III, Protein C, Protein S
á Suspicions for anticardiolipin antibodies or lupus anticoagulant
á Strong family history of clotting disorder and unprovoked clots.
o For DVT: Doppler ultrasound with compression is imaging of choice.
¤ If inconclusive, further studies may include MRI, venogram
o For PE: Spiral CT has sensitivity 70-90%. Excellent negative predictive value
¤ Most pts w/ PE will have an abnormality on CXR but this is non-specific
¤ Echo: useful when concern for massive PE that requires thrombolysis: looking for elevated RV Pressure or RV strain
á Treatment
o Thrombolytic therapy (tPA): use if hemodynamic compromise, RV strain, severe hypoxia associated with PE.
¤ Consider if large extremity clot.
¤ Many contraindications. Significant risk of bleeding as a complication.
o Interventional thrombectomy/thrombolysis. Consider for massive PE, extremity compromise.
o Anticoagulant therapy: to prevent thrombus growth, remodel current thrombus
¤ Initial treatment of choice: Low-molecular weight heparin (Lovenox)
á Follow platelets due to risk of heparin-induced thrombocytopenia
á Unfractionated heparin rarely used but an option
¤ Options after initial anticoagulation
á Continue LMWH or Heparin
á Transition to warfarin (Coumadin)
á Transition to direct oral anticoagulant (dabigatran, rivaroxaban)
o Not yet approved in pediatrics, expensive, no reversal agent
o Avoid aspirin, NSAIDs, high impact activities.
o Compression stockings to prevent post thrombotic syndrome (if extremity clot).
Lovenox dosing
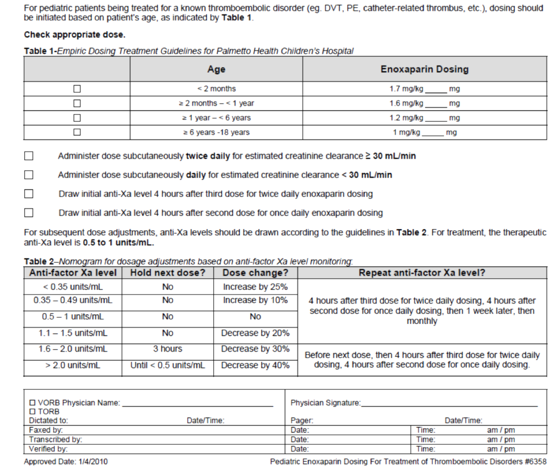
Bleeding Disorders
á
ITP: Immune
Thrombocytopenic Purpura
o Etiology: autoimmune. Antibodies ˆ faster clearing of plts by macrophages ˆ shortened lifespan, lower numbers.
¤ Most common ages: 2-7 yrs
o Manifestations: bruising, petechiae most often. Can have major bleeds such as intracranial hemorrhage, commonly follows a viral illness, occasionally immunizations
o Lab: isolated thrombocytopenia with large platelets.
¤ Plts usually <100K to fit diagnosis. Most often <30K
o Exam: petechiae, purpura, bruising, oral petechiae, wet purpura
¤ Some may have slightly enlarged spleen
¤ Otherwise very well-appearing
o Course: most often resolves spontaneously within 3-6 months
¤ Few cases become chronic
¤ 3% will have serious bleed (severe epistaxis, GI bleed, ICH)
¤ <1% will have intracranial hemorrhage (most are supratentorial)
o Treatment
¤ Patients with no bleeding or mild bleeding, regardless of platelets
á NO pharmacologic treatment
á Avoid contact sports, activities with bleeding risk, ibuprofen, aspirin
¤ Patients with ICH or severe bleeding causing anemia requiring transfusion
á IVIG 1 g/kg x1-2 doses OR
á IF Rh+, RhoGAM (anti-D immune globulin) but has black box warning
á Strongly consider adding steroids to IVIG for ICH or severe bleeding.
á If suspect SLE do labs before IVIG
¤ Other treatments:
á Steroids: should consider need to r/o bone marrow pathology (malignancy!) before use. Must discuss with Heme-Onc first.
á Platelet transfusions: do not help except in extreme circumstances. Transfused platelets will be cleared by the same mechanism as native platelets.
á Plasmapheresis: transient benefit. Not commonly used.
¤ Consider in chronic ITP:
á Splenectomy: will increase plt count in 80% of patients. Use conservative measures first as this is major surgery and leaves patient immunocompromised. Will need pre-op immunizations for encapsulated bacteria.
á Thrombopoietin receptor agonists (eltrombopag, romiplostim). High dose Dexamethasone:
á Immunosuppresion (Rituximab and others)
á Disseminated Intravascular Coagulation
o Definition: an acquired syndrome of microvascular coagulation and hemorrhage
o Etiology:
¤ Many potential triggers for endothelial damage, activation of clotting:
á Sepsis, toxins (rattlesnake bites), malignancy, trauma/tissue injury, burns, collagen vascular disease, liver disease (Reye Syndrome)
¤ endothelial damage triggers coagulation cascade ˆ fibrin formed in vessels ˆ fibrinolysis occurs simultaneously.
¤ coagulation factors consumed and clots form ˆ micro-thrombi form and hemorrhage occurs in absence of available coagulation factors
¤ Thrombi lead to organ damage
¤ Fibrin strands across blood vessels lead to hemolysis (schistocytes)
o Manifestations:
¤ Bleeding: bruising, petechiae, purpura, oozing from IV sites, gross hemorrhage in an ill child
¤ Signs of micro-embolism: acral gangrene
o Lab findings:
¤ Anemia with red cell fragmentation (schistocytes on smear)
¤ Platelets <100K
¤ Prolonged PT/PTT
¤ Elevated D-dimer and fibrin degradation products
¤ Fibrinogen <200 in acute DIC (can be normal in chronic DIC)
o Treatment
¤ Definitive treatment is to address the underlying condition
¤ Supportive care to normalize coagulation:
á FFP 10 cc/kg x1, can repeat PRN Q12-24 hrs. Goal is to stop bleeding, not to normalize labs
á Cryoprecipitate 1 bag /5-10 kg if fibrinogen extremely low or if volume overload an issue with FFP. Usually start with at least 1 dose of FFP first.
á Platelets can be given as well but will raise the plt count less than expected since they will be consumed in DIC as well
¤ Anticoagulation with heparin/LMWH if significant thrombosis that must be reversed. Not commonly done. Controversial due to bleeding risk.
á
Hemophilia
A or B
o
Etiology: X-linked recessive deficiency of
Factor VIII (A) or FIX (B)
¤
Normal PT, prolonged aPTT.
¤
aPTT will correct in
mixing studies.
¤
Factor FVIII or FIX levels are low
o
Manifestations: Bleeding in soft tissues,
joints, or excessive bleeding from minor trauma (IV stick, fingerprick)
¤
Severe: <1% of factor VIII/IX activity.
Presents in first few months. Many with large cephalohematoma, subgaleal
hematoma at birth or prolonged bleeding from circumcision
¤
Moderate: 1-5% of factor VIII/IX activity.
Presents at average 6-9 months, often with MSK bleeding
¤
Mild: 6-40% of factor VIII/IX activity. Presents
at 1-3 years or later, often with MSK bleeding or post op /trauma related
bleeding.
o
Treatment: 1 unit of factor VIII per kg raises
factor level by 2%. 1 unit of FIX raises factor levels 1%.
¤
Chronic treatment: goal is to maintain factor
level at >1% or higher to prevent major hemorrhage
¤
For urgent/emergent treatment:
|
Desired Factor Activity Levels for
Specific Situations |
|
|
Type of Hemorrhage |
Desired Factor Level |
|
Life Threatening Bleeds
|
100% |
|
Spontaneous Joint Bleed |
40-60% |
|
Spontaneous Muscle Bleed |
40-60% |
|
Severe Abdominal Pain |
40-80% |
|
Simple Dental Extraction |
40% |
*Remember, in some instances may need to achieve higher levels and may need repeated doses. Should use recombinant FVIII or FIX concentrates and NOT plasma derived concentrates or cryoprecipitate unless that is what the patient normally uses or for extreme emergencies or recombinant products are not available. There are now many products available and a good rule of thumb is to use the patientÕs home supply if possible.
If the patient has an inhibitor then he may not be able to use a factor concentrate or may need an increased dose. Consult Hematology.
á Von Willebrand Disease
o Etiology
¤ Low(type 1) or absent (type 3) von Willebrand factor levels
¤ Dysfunctional VWF protein (type 2)
¤ Usually autosomal dominant inheritance. Typically has a family history.\
o Clinical history:
¤ Mucocutaneous bleeding, post-traumatic bleeding
¤ Menorrhagia from the time of menarche
¤ Types 2, 3 can have deep MSK bleeds, hemarthrosis
o Lab findings:
¤ Usually Ristocetin CoFactor Activity(RCO) and/or vW Antigen is low, FVIII may be low
¤ PTT may be elevated, Platelet Function Screen may be elevated. Plts can be low.
o Treatment: Most type 1 and some type 2 is DDAVP +/- antifibrinolytic (Episilon –amino caproic acid or Tranexamic acid)
¤ Most type 2 and all type 3 (some severe or non-DDAVP responsive type 1) get von Willebrand factor containing concentrate: Humate P, Alphanate Wilate or recombinant vW factor concentrate +/- antifibrinolytic.
¤ May need to follow RCO or Antigen levels
¤ If using DDAVP, fluid restrict to maintenance only for 12-24 hours after each dose and use no more than 3 consecutive daily doses as tachyphylaxis may occur.
¤ Can consider monitoring sodium levels for extremes of age and patients who get more fluids (ie post op) as it can lead to hyponatremia and seizures.
Appendix
Quick Calculations
Blood Pressure Norms
|
Percentile for age (over 2 years
old) |
Systolic (mmHg) |
Diastolic (mmHg) |
|
<5th |
70 + (2 x age in years) |
|
|
50th |
90 + (2 x age in years) |
70 + (1.5 x age in years) |
|
95th |
100 + (2 x age in years) |
70 + (2 x age in years) |
Glucose Infusion Rate
GIR in mg/kg/min = (%dextrose x 10 x rate of infusion (ml/hr))/ 60 x wt in kg
Serum Osmolality
Serum osm= 2(Na) + (BUN/2.8) + (Glucose/18)
Adjusted Sodium for
Hyperglycemia
Adjusted Na = Na x 1.6 (glucose/100 -1)
Body Surface Area
Body surface area (actual) = square root of [wt (kg) x ht (cm)]/3600
Body surface estimated = [(wt(kg) x 4) +7] / (wt + 90)
Fractional Excretion
of Sodium
FENa = (Urine Na x Serum Cr) x 100
(Urine Cr x Serum Na)
Estimated total blood volume: 70 cc/kg body weight
IVIG Administration Protocol
- Dosing:
- ITP – 1 gram/kg
- Kawasaki Disease – 2 grams/kg
- Stevens-Johnson – 2 grams/kg
- Pre-medication with Tylenol and Benadryl reduces side effects
- Side effects include: fatigue, chills, muscle aches/cramps, fever, urticaria, pruritis, nausea, vomiting
- Serious (rare) side effects: anaphylaxis (IgA deficient patients at risk), aseptic meningitis, hemolytic anemia, non-infectious hepatitis
- Using large veins if possible reduces infusion site pain.
- Initiate slowly and increase rate as below. This reduces risk of flushing, hypotension.
- If these symptoms occur, slow or stop the infusion for 30-60 min.
Infusion rates:
0.5ml/kg/hr x 30 minutes, then
1ml/kg/hr x 30 minutes, then
2ml/kg/hr x 30 minutes, then
4ml/kg/hr end of infusion
Check vital signs:
Every 15 minutes x 1 hour, then
Every 30 minutes x 2 hours, then
Every hour until complete